Psoriasis Treatment Timeline Calculator
Treatment Timeline Simulator
This tool shows what to expect during methylprednisolone treatment for psoriasis. It visualizes symptom improvement, potential side effects, and tapering schedule based on your treatment plan.
Your Treatment Journey
When doctors need a fast‑acting anti‑inflammatory, Methylprednisolone is a synthetic glucocorticoid that calms an over‑active immune response and cuts swelling. That makes it a useful tool for people struggling with severe psoriasis, a skin condition that thrives on inflammation. Below you’ll learn exactly how this drug works, when it’s prescribed, what to watch for, and how it stacks up against other systemic options.
What Is Methylprednisolone?
Methylprednisolone belongs to the glucocorticoid class of hormones. It mimics cortisol, the body’s natural stress hormone, and binds to glucocorticoid receptors in almost every cell. The binding triggers a cascade that suppresses the production of inflammatory chemicals like prostaglandins and cytokines.
Because it works systemically-meaning it travels through the bloodstream-it can reach deep‑seated immune cells that topical creams can’t touch. That’s why dermatologists sometimes choose it for plaque‑type psoriasis that covers large body areas or resists topical treatment.
Why Psoriasis Flare‑Ups Happen
Psoriasis is driven by a mis‑firing immune system. T‑cells release excess inflammation signals, prompting skin cells to multiply 10‑times faster than normal. The result: thick, red, scaly patches that itch and can crack.
Genetics set the stage, but triggers like stress, infections, or certain medications can tip the balance. When the immune attack intensifies, patients notice more surface area involved, thicker plaques, and higher discomfort.
When Doctors Choose Methylprednisolone for Psoriasis
Systemic steroids are not first‑line for chronic psoriasis because long‑term use can cause rebound flare‑ups once the drug stops. However, they shine in specific scenarios:
- Acute worsening: Sudden, extensive eruptions that impair daily activities.
- Pregnancy‑related flares: When safer options are limited.
- Co‑existing inflammatory conditions: Such as severe asthma or rheumatoid arthritis, where a single drug can address multiple issues.
In these cases, a dermatologist will prescribe a short, high‑dose course to gain rapid control, then taper down to avoid rebound.
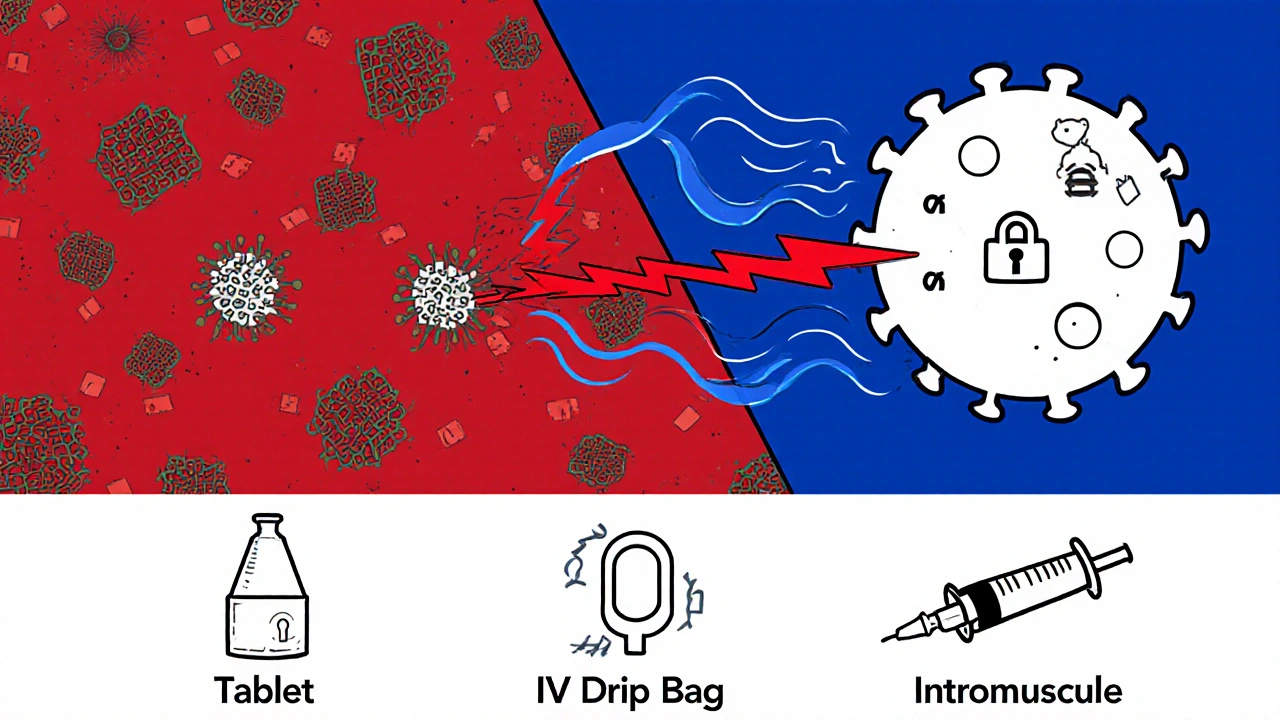
Typical Dosing & Administration
The exact dose depends on severity, body weight, and whether the drug is given orally, intravenously, or as an intramuscular injection. Common regimens include:
| Route | Typical Dose | Frequency | Onset of Relief |
|---|---|---|---|
| Oral tablets | 16-48 mg | Once daily | 2-3 days |
| IV infusion | 1-2 mg/kg | Single burst | Within hours |
| IM injection | 40-80 mg | Every 2-3 days | 1-2 days |
Doctors usually start with the lowest effective dose and monitor blood pressure, blood sugar, and mood changes. After the skin clears enough, they taper the dose gradually-often over 2‑4 weeks-to give the body’s adrenal glands time to resume natural cortisol production.
Benefits Patients Notice
- Rapid itch reduction: Most people feel less itching within 48‑hours.
- Plateau‑flattening: Thick plaques soften and shrink quicker than with topical steroids alone.
- Improved quality of life: Less scaling means fewer cracks, less pain, and better sleep.
Because the effect is fast, patients often report a psychological lift-confidence returns when the visible signs recede.
Potential Side Effects & Safety Tips
Even short courses can cause unwanted reactions. Common issues include:
- Elevated blood sugar - watch if you have diabetes.
- Increased blood pressure - keep an eye on readings.
- Mood swings or insomnia - report severe anxiety or depression.
- Weight gain and facial rounding - usually linked to longer use.
- Suppressed adrenal function - why tapering is critical.
To stay safe, follow these practical steps:
- Take the drug exactly as prescribed; never self‑adjust the dose.
- Schedule regular check‑ins with your dermatologist to track progress.
- Maintain a food diary if you have diabetes - note any spikes.
- Keep a symptom journal for mood or sleep changes.
- Never stop abruptly; follow the taper plan your doctor provides.
How Methylprednisolone Stacks Up Against Other Systemic Options
| Drug | Class | Onset | Typical Duration | Key Risks |
|---|---|---|---|---|
| Methylprednisolone | Glucocorticoid | Hours‑days | Weeks (short‑term) | Adrenal suppression, rebound flare |
| Prednisone | Glucocorticoid | Days | Weeks | Similar steroid‑specific risks |
| Cyclosporine | Calcineurin inhibitor | Weeks | Months‑years | Kidney toxicity, hypertension |
| Methotrexate | Antimetabolite | Weeks | Months‑years | Liver damage, marrow suppression |
| Biologic (e.g., IL‑17 inhibitor) | Targeted immunotherapy | Weeks | Years | Infection risk, high cost |
If you need quick relief, a steroid burst wins on speed. For long‑term control, doctors usually transition to biologics or other disease‑modifying agents after the steroid taper.
Practical Checklist Before Starting Therapy
- Confirm diagnosis with a skin biopsy if uncertain.
- Review medical history - especially diabetes, hypertension, or psychiatric conditions.
- Discuss pregnancy plans - steroids cross the placenta.
- Ask about vaccination status - live vaccines should be avoided during high‑dose therapy.
- Set up baseline labs: CBC, CMP, fasting glucose, and blood pressure.
Having this information ready makes the first appointment smoother and helps the dermatologist tailor the regimen.
Frequently Asked Questions
Can I use methylprednisolone forever for psoriasis?
No. Long‑term steroid use can cause skin thinning, adrenal suppression, and rebound flare‑ups. It’s meant for short bursts, followed by a taper and transition to non‑steroid systemic or biologic therapy.
How quickly will I see improvement?
Most patients notice less itching and softer plaques within 2‑3 days of oral dosing. Full flattening can take a week or two, depending on severity.
What are the signs that I need to stop the medication?
Severe mood changes, uncontrolled high blood sugar, sudden swelling of the face or limbs, or signs of infection (fever, chills) should prompt an immediate call to your doctor. Never stop abruptly without a taper plan.
Is methylprednisolone safe during pregnancy?
It’s classified as Category C - meaning risk can’t be ruled out. Doctors only prescribe it if the benefits outweigh potential fetal risks, usually for severe flares that other drugs can’t manage.
Will my skin become dependent on steroids?
Dependence can happen if steroids are used continuously for months. That’s why a short‑term plan with clear tapering is essential. After stopping, most patients stay clear or move to a maintenance drug.
Overall, methylprednisolone offers a fast‑acting bridge for people whose psoriasis suddenly flares. Pairing it with a solid taper schedule, regular monitoring, and a plan for long‑term therapy can turn a painful breakout into a manageable episode.
Ron Lanham
October 20, 2025 AT 21:06When it comes to the reckless reliance on quick fixes for chronic skin diseases, we must first acknowledge the ethical responsibility each physician bears toward their patients. The temptation to prescribe a high‑dose glucocorticoid like methylprednisolone without a thorough discussion of long‑term consequences is a moral failing that betrays the trust inherent in the doctor‑patient relationship. Steroids, while undeniably potent, are a double‑edged sword; they can quench the fury of an uncontrolled immune assault, but they also pave the way for adrenal suppression and catastrophic rebound flares if misused. It is incumbent upon us to scrutinize every indication, ensuring that the drug is reserved for truly acute, debilitating episodes that cannot be managed by safer modalities. The literature is clear: short courses may provide rapid relief, yet the moment the taper is omitted or the dosage is prolonged, patients are plunged into a vicious cycle of dependence. Moreover, we must not overlook the psychosocial dimension-patients often experience a false sense of security, believing that the steroid will be a permanent panacea. This illusion can lead to neglect of essential lifestyle modifications, such as stress management and dietary vigilance, which are pivotal in sustaining remission. The prescribing clinician should therefore act as an educator, demystifying the pharmacodynamics while candidly presenting the spectrum of possible adverse effects, from hyperglycemia to mood disturbances. In doing so, we empower patients to become active participants in their own care rather than passive recipients of a fleeting remedy. The principle of “first, do no harm” is not an antiquated platitude but a directive that must guide every therapeutic decision, especially when dealing with potent agents like methylprednisolone. Finally, a multidisciplinary approach-integrating dermatology, endocrinology, and mental health services-ensures that the short‑term gains do not eclipse the long‑term well‑being of the individual. To summarize, the judicious, time‑limited use of methylprednisolone can be life‑changing, but only when embedded within a comprehensive, ethically grounded treatment plan.
Andrew Hernandez
October 26, 2025 AT 15:46Appreciate the thorough overview here it really helps understand when steroids are truly needed and how to manage them responsibly
Alex Pegg
November 1, 2025 AT 11:30Honestly steroids feel like a crutch when you could be tackling the root causes.
laura wood
November 7, 2025 AT 07:13I totally get how scary the side effects can sound, especially for people already dealing with a lot. It’s comforting to know that with proper monitoring and a clear taper plan, the risks can be minimized and you can get back to feeling like yourself sooner rather than later.
Kate McKay
November 13, 2025 AT 02:56Great info! Just remember to keep a diary of any mood swings or blood sugar spikes. It makes the follow‑up appointments much more productive and helps your doctor fine‑tune the dose.
JessicaAnn Sutton
November 18, 2025 AT 22:40The article correctly delineates the pharmacokinetic profile of methylprednisolone, highlighting its rapid onset of action relative to other systemic agents. Nevertheless, it understates the immunosuppressive burden that even brief courses impose on patients with latent infections. A meticulous risk‑benefit analysis, preferably documented in the electronic health record, is indispensable prior to initiation. Moreover, the tapering schedule should be individualized based on hypothalamic‑pituitary‑adrenal axis recovery metrics rather than a one‑size‑fits‑all protocol. Finally, comparative effectiveness research remains sparse; clinicians must therefore rely on pragmatic clinical judgment when transitioning to long‑term biologic therapy.
Sebastian Green
November 24, 2025 AT 18:23Thanks for sharing this. It’s helpful to see the practical steps laid out in one place.
Wesley Humble
November 30, 2025 AT 14:06While the overview is comprehensive, one must underscore that the systemic exposure of methylprednisolone can precipitate iatrogenic Cushingoid features, especially in patients with underlying metabolic syndrome. 📈 It is advisable to schedule periodic endocrinological assessments to preempt potential dysregulations. 🙏
barnabas jacob
December 6, 2025 AT 09:50Look bro, the steroid hype is overblown if u dont watch ur labs and stay on the low‑dose protocol. Dont be that guy who just ramps up and crashes hard.
jessie cole
December 12, 2025 AT 05:33Remember, the journey from acute flare to stable skin is a marathon, not a sprint. Stay vigilant, follow the taper, and you’ll emerge stronger.
Kirsten Youtsey
December 18, 2025 AT 01:16One must also consider the pharmaceutical lobby’s role in promoting steroids as the first‑line emergency solution-it is not a coincidence that such narratives dominate mainstream discourse.







11 Comments