When your hip starts hurting, it’s easy to blame aging, overuse, or a bad workout. But if the pain is deep, sharp, or gets worse when you sit, squat, or twist, it might be something more specific: a labral tear or early hip arthritis. These aren’t just random injuries - they’re linked. And how you move every day can either make them worse… or help you live with them without surgery.
What’s Actually Going on in Your Hip?
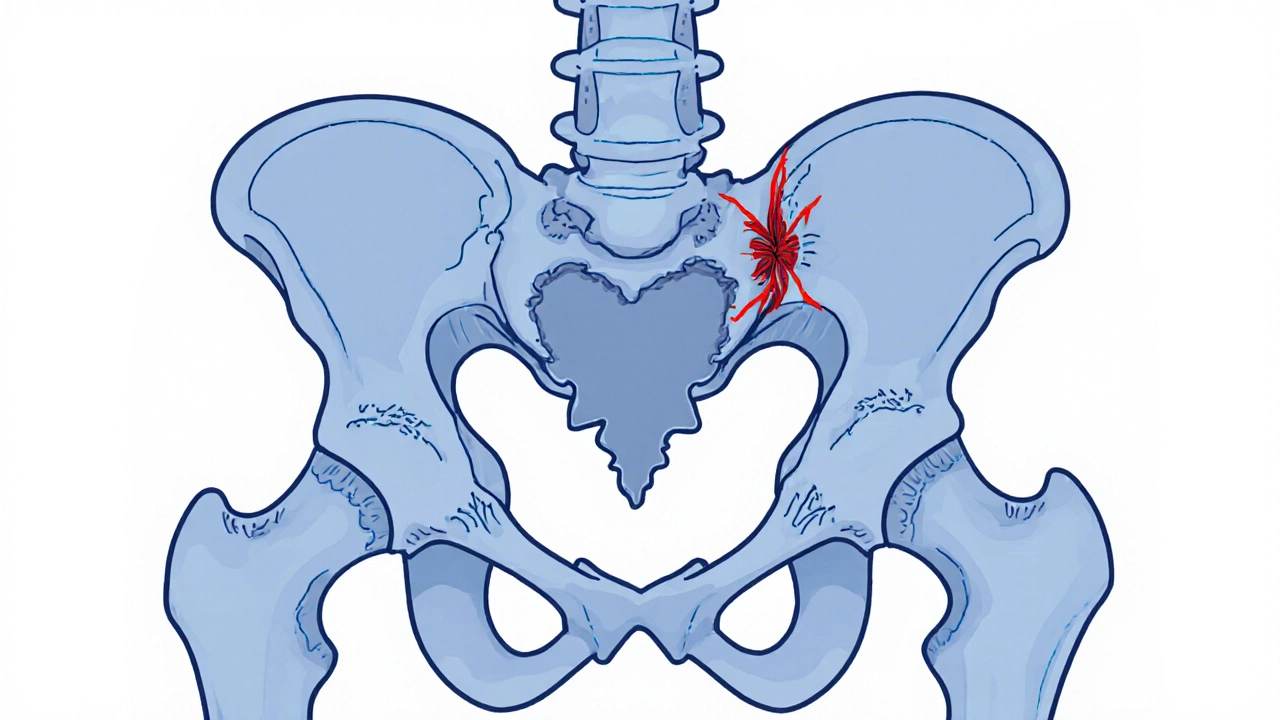
Your hip joint is a ball-and-socket. The ball is the top of your thigh bone. The socket is your pelvis, lined with a ring of tough cartilage called the labrum. This labrum is about 3 to 5 millimeters thick - thin, but critical. It acts like a rubber seal, keeping joint fluid inside so your bones glide smoothly. When it tears, that seal breaks. Stress spikes inside the joint. Cartilage starts wearing faster. That’s how a labral tear can lead to arthritis - not the other way around, always. Hip arthritis, or osteoarthritis, is the slow breakdown of that smooth cartilage covering the bones. It’s not just "wear and tear." It’s a chemical and mechanical cascade. Once cartilage starts thinning, bone rubs on bone. Bone spurs form. The joint swells. Pain gets constant, not just after activity. The scary part? These two problems often show up together. Studies show 70 to 90% of people with a type of hip impingement called FAI (femoroacetabular impingement) have a labral tear. And over half of people with hip arthritis also have a torn labrum - even if they never had a fall or injury. That’s because the labrum is the first thing to fail when the joint’s alignment is off.Labral Tears: More Common Than You Think
Most labral tears aren’t from accidents. They come from how your hip is built. Two main shapes cause trouble:- Cam-type impingement: A bump on the ball of your thigh bone rubs against the socket. This is the most common - about 64% of cases. It’s often seen in athletes, especially soccer players, dancers, or hockey players.
- Pincer-type impingement: The socket is too deep or covers too much of the ball. This crushes the labrum over time. More common in women.
Arthritis: The Silent Progression
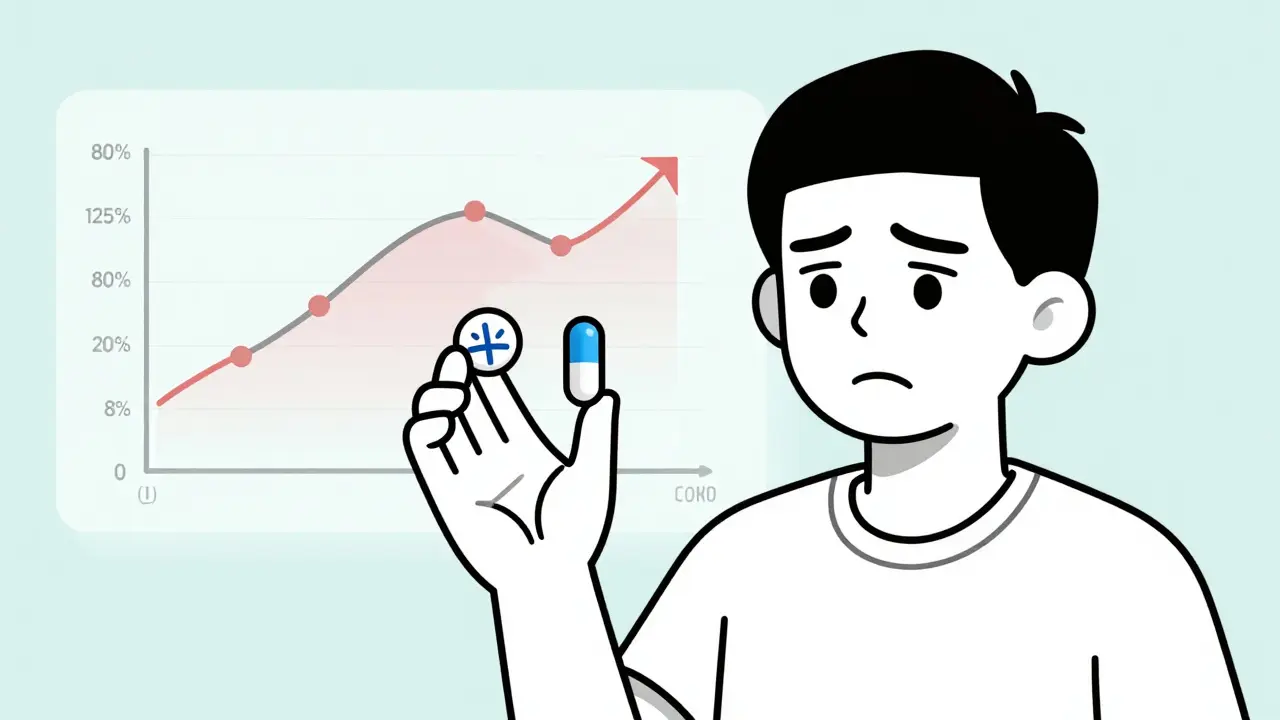
Hip arthritis doesn’t show up overnight. It follows the Kellgren-Lawrence scale, from Grade 0 (no change) to Grade 4 (bone on bone). Most people don’t realize they’re in Grade 2 or 3 until the pain hits hard. By the time you’re 65, 30% of Americans have noticeable hip arthritis. But not everyone needs surgery. Many can manage for years - if they change how they move. The key difference between labral tears and arthritis? Labral tears often respond well to repair. Arthritis doesn’t reverse. But you can slow it. A lot.Activity Modification: The Real Game-Changer
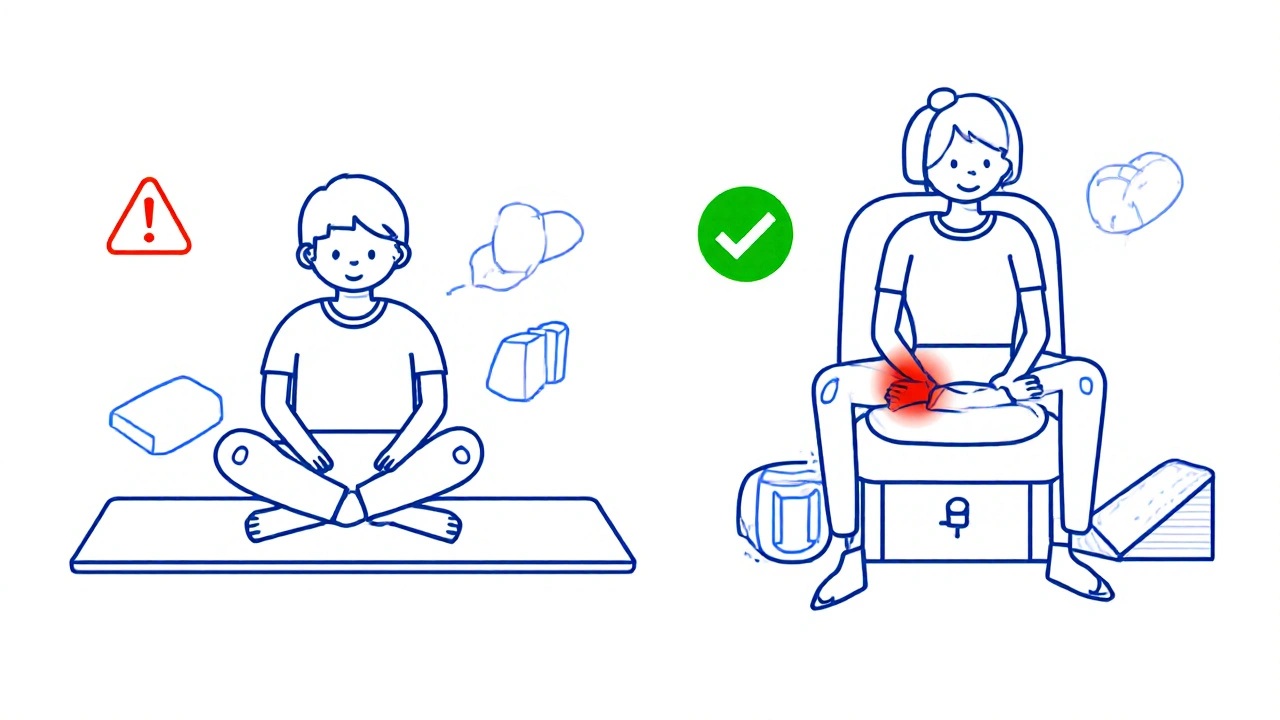
You don’t need to stop moving. You need to move smarter. Here’s what works, based on real patient data from clinics in Sydney, Boston, and Minneapolis:- Don’t sit with your knees higher than your hips. That’s cross-legged sitting, deep squats, or low couches. Keep your hips above your knees. Use a pillow under your seat if needed.
- Avoid twisting your hip while bent over. That’s putting on socks, tying shoes, or reaching for something low. Bend your knees, not your hips. Use a reacher tool if you have to grab things off the floor.
- Stop deep squats and lunges. These force the hip into flexion and internal rotation - the exact position that grinds a torn labrum. Swap them for glute bridges, step-ups, or leg presses with limited range.
- Use a wedge cushion in your car. Sitting for long drives? A 10- to 15-degree wedge reduces hip flexion. It’s simple, cheap, and backed by motion analysis studies.
- Sleep with a pillow between your knees. This keeps your hips aligned and stops your leg from rolling inward at night - a silent pain trigger.
- Choose low-impact cardio. Swimming and elliptical trainers are gold. Running? 71% of people with hip pain quit it. Cycling? Only if your saddle is high enough to avoid deep hip flexion.
What Doesn’t Work (And Why)
Painkillers? They mask pain, not the problem. NSAIDs like ibuprofen help temporarily, but don’t stop cartilage loss. And overuse can damage your stomach or kidneys. Cortisone shots? They give 3 to 4 months of relief for about 68% of people. But if you get more than three a year, you risk damaging the cartilage even faster. They’re a pause button, not a fix. Viscosupplementation (hyaluronic acid injections)? They add joint fluid. Sounds smart. But studies show only 55% of people get 15-20% pain reduction - and it fades after six months. Not worth it for most. Surgery? Hip arthroscopy to repair a labral tear works well - 85-92% of people under 50 report satisfaction after five years. But if you already have Grade 3 or 4 arthritis, surgery won’t help. You’ll need a hip replacement eventually anyway. And that’s a major operation with a long recovery.When to Consider Surgery - And When Not To
Surgery makes sense if:- You’re under 50
- You have a clear cam-type impingement (alpha angle >55° on MRI)
- Your pain is sharp, not dull, and limits daily life
- You’ve tried 3-6 months of physical therapy and activity changes
- You’re over 60 with bone-on-bone arthritis
- Your pain is constant, even at rest
- Your X-ray shows joint space narrowing under 2mm
- You have other health issues that make recovery risky
The Invisible Disability
One of the hardest parts? People don’t get it. You look fine. No cast. No crutches. But you can’t sit through a movie. You can’t play with your kids on the floor. You avoid stairs. You skip family dinners because the chairs are too low. A survey from the Hospital for Special Surgery found 68% of people with hip labral tears felt misunderstood. "They think I’m lazy," one 38-year-old teacher said. "I’m not. I just can’t move like I used to." That’s why education matters. Not just for you - for your family, your boss, your gym coach.Real People, Real Changes
A 45-year-old yoga instructor in Sydney stopped doing pigeon pose and deep forward folds. She started using blocks to keep her hips above her knees. Within three months, her pain dropped 70%. She’s still teaching - just differently. A 52-year-old accountant switched from sitting all day to standing every 30 minutes. He bought a footrest. He now uses a raised toilet seat. His pain went from 7/10 to 2/10. A 34-year-old cyclist swapped road biking for swimming. He lost 15 pounds. His hip pain vanished. He didn’t need surgery. These aren’t miracles. They’re adjustments.What’s New in 2025
New tools are helping people manage hip pain better:- Wearable sensors: Tiny devices you stick to your hip track how you move during the day. They buzz when you flex too far. A Stanford pilot study showed a 52% drop in pain episodes over 12 weeks.
- Longer-lasting injections: Durolane, a new hyaluronic acid shot, lasts up to six months - twice as long as older versions.
- Quantitative MRI: New scans can see cartilage thinning before it shows up on regular X-rays. This helps catch problems earlier.
Your Action Plan
If your hip hurts, here’s what to do next:- Track your pain triggers. Write down what makes it worse: sitting? climbing? twisting?
- Start activity modification today. Pick three changes from the list above and stick with them for 4 weeks.
- See a physical therapist who specializes in hips. They’ll teach you how to move without grinding your joint.
- Get an X-ray and possibly an MRI - but only if your symptoms match the imaging. Don’t get scanned just because you’re in pain.
- Don’t rush to surgery. Try 6 months of conservative care first. Most people improve.
Can a labral tear heal on its own?
No. The labrum has very little blood supply, so it doesn’t heal like a muscle or ligament. But you can stop it from getting worse. By changing how you move, you reduce the stress on the tear. Many people live pain-free without surgery by avoiding positions that aggravate it.
Is walking good for hip arthritis?
Yes - if you do it right. Walk on flat surfaces. Avoid hills and stairs if they hurt. Wear supportive shoes. Keep your stride short and your hips aligned. Walking 20-30 minutes a day helps maintain joint fluid and muscle strength. But if walking causes pain that lasts more than two hours after, you’re doing too much.
Should I stop exercising if my hip hurts?
No. Stopping movement leads to muscle loss, which makes your hip less stable and more painful. Instead, switch to low-impact activities: swimming, cycling (with high seat), elliptical, or water aerobics. Focus on strengthening your glutes and core - they support your hip. A physical therapist can design a safe program.
Does weight loss help hip pain?
Absolutely. Every pound of body weight adds 3-4 pounds of pressure on your hip with each step. Losing just 10 pounds can reduce hip pain by 20-30%. It’s not a cure, but it’s one of the most effective ways to slow arthritis and reduce strain on a torn labrum.
How long does activity modification take to work?
Most people notice less pain in 3 to 6 weeks. Full improvement takes 3 to 6 months. It’s not instant. But if you stick with it, you’ll build new movement habits that protect your hip for years. The key is consistency - not perfection.
Can I still run with a labral tear?
It’s risky. Running creates high-impact forces that can worsen a tear and speed up cartilage damage. Most people with labral tears who keep running end up needing surgery sooner. If you want to run, switch to a treadmill with shock absorption, shorten your stride, and limit runs to 2-3 times a week. But many find swimming or cycling just as effective - and much kinder to the hip.
What’s the best sleeping position for hip pain?
Sleep on your back with a pillow under your knees - or on your side with a pillow between your knees. This keeps your hips aligned and stops your leg from rolling inward, which can pinch the labrum. Avoid sleeping on the painful side if it worsens pain. A firm mattress helps too.
Can physical therapy fix a labral tear?
It won’t heal the tear, but it can fix the muscle imbalances that make the tear painful. Strengthening your glutes, hips, and core reduces pressure on the joint. Many patients avoid surgery entirely after 8-12 sessions of targeted therapy. Physical therapy is the first step - not a last resort.




10 Comments