CGM Trend Arrow Insulin Calculator
Use this tool to calculate the correct insulin adjustment based on your CGM trend arrows and personal correction factor. Follows Endocrine Society guidelines for safe, proactive dosing.
Adjustment Result
When your glucose is dropping fast and you’re about to eat, should you take your full insulin dose? What if your sugar is climbing even though you didn’t eat anything? These aren’t hypotheticals-they’re daily decisions for people using continuous glucose monitors (CGMs). The real power of CGM isn’t just seeing your number. It’s seeing where it’s going. And that changes everything about how you take your diabetes meds.
What CGM Trend Arrows Actually Tell You
Your CGM doesn’t just show your current glucose level. It shows you the direction and speed of change with arrows: up, down, flat, or double up/down. These aren’t decorative. They’re predictive signals. A single-up arrow means your glucose is rising about 1-2 mg/dL per minute. A double-down arrow? That’s falling faster than 2 mg/dL per minute-likely heading into hypoglycemia in 15-30 minutes if nothing changes.
These trends come from real-time data collected every 5 minutes. Unlike a fingerstick that gives you a single snapshot, CGM shows you the story. And that story lets you act before the problem happens. That’s why the Endocrine Society published formal guidelines in 2017: use those arrows to adjust insulin doses proactively, not reactively.
How to Adjust Insulin Based on Arrows (The Proven Method)
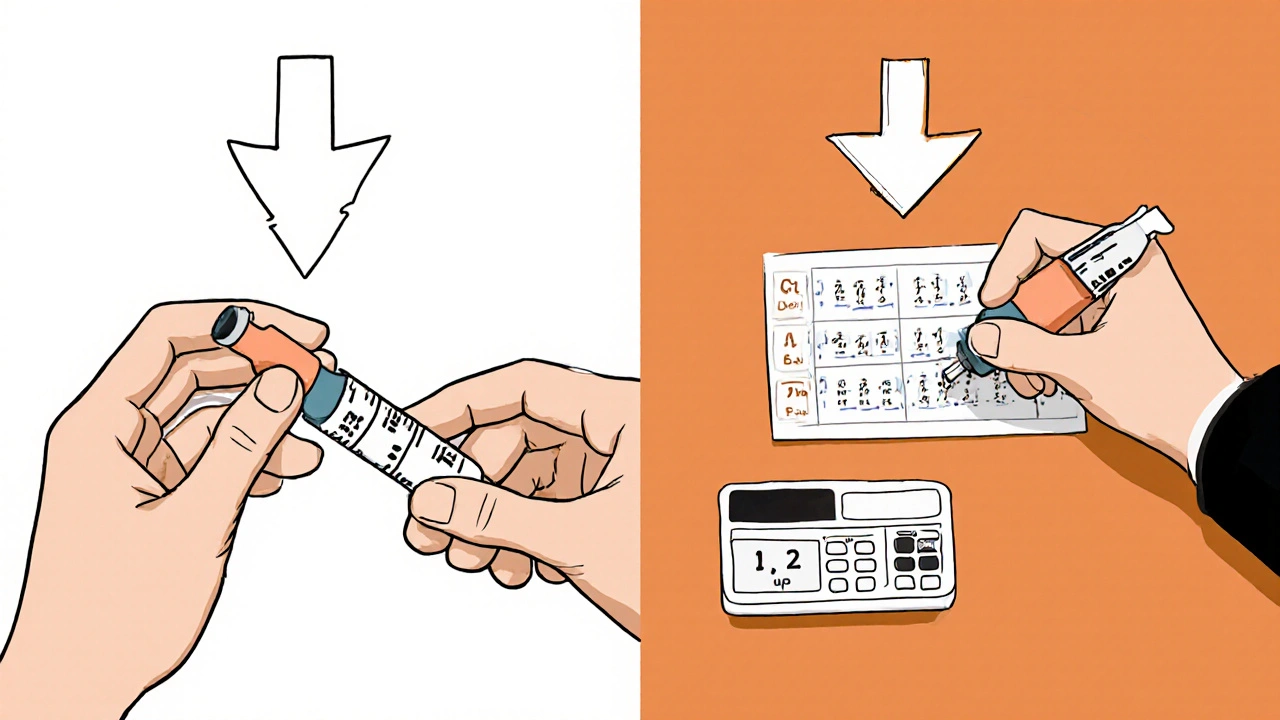
The standard approach comes from the Endocrine Society’s 2017 guidelines, validated in clinical trials and now used by diabetes educators worldwide. It’s simple: you don’t guess. You use your personal correction factor and follow fixed unit adjustments based on the arrow.
First, know your correction factor. That’s how much one unit of insulin lowers your blood sugar. For example, if your correction factor is 1:50, one unit drops your glucose by 50 mg/dL. If it’s 1:30, one unit drops it by 30 mg/dL. Most adults fall between 1:30 and 1:60. Your provider should have helped you figure this out.
Now, here’s the adjustment table for adults:
- Double-up arrow (fast rising): Add 1.2 units to your pre-meal or correction dose
- Single-up arrow (rising): Add 0.8 units
- Flat arrow (stable): No change
- Single-down arrow (falling): Subtract 0.8 units
- Double-down arrow (fast falling): Subtract 1.2 units
For kids and teens, the adjustments are smaller: +1.0, +0.6, 0, -0.6, -1.0 units respectively. These numbers aren’t arbitrary. They’re based on average insulin sensitivity and glucose kinetics. They eliminate guesswork. You don’t need to calculate percentages. You just match the arrow to the number.
Important: These adjustments are for pre-meal boluses and correction doses given more than 3 hours after eating. Don’t adjust for meals you just ate-you’re already covered by your carb ratio.
Why This Works Better Than Old Methods
Before CGMs, people adjusted insulin based on a single number and how they felt. If your sugar was 220, you took your usual correction. But what if it was already falling? You could end up with a low. If it was 80 and rising fast? You might wait too long to act.
A 2017 study in Diabetes Technology & Therapeutics showed people using trend arrows had 28% fewer hypoglycemic events and spent 17% more time in target range than those using only fingersticks. Why? Because you’re not treating a past number-you’re preventing a future one.
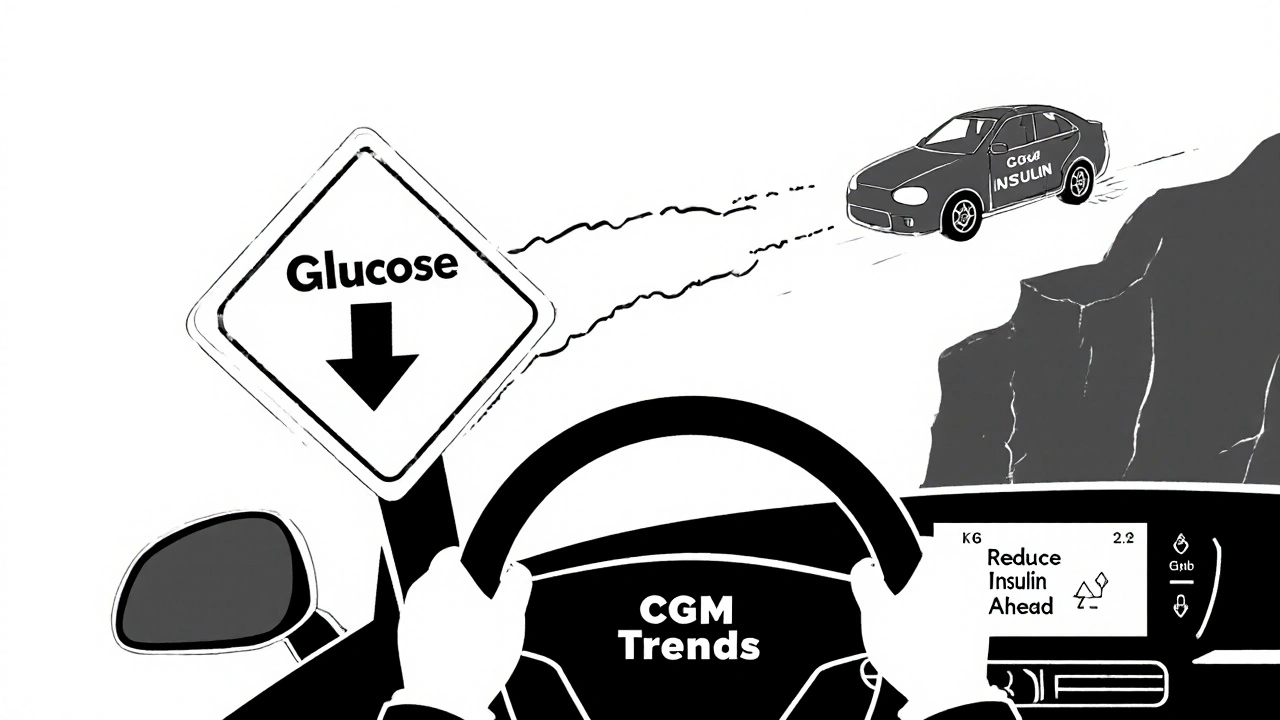
Think of it like driving. A fingerstick is like checking your speedometer once every 10 minutes. A CGM with arrows is like having a GPS that tells you you’re accelerating toward a cliff. You don’t wait until you hit it. You brake early.
What About Non-Insulin Medications?
Most people think CGM adjustments only apply to insulin. But that’s changing. The 2024 ADA/EASD consensus report now recommends adjusting SGLT2 inhibitors (like dapagliflozin or empagliflozin) when CGM shows persistent euglycemic ketosis: glucose under 180 mg/dL with ketones above 0.6 mmol/L.
Why? Because SGLT2 inhibitors can cause ketones to build up even when glucose is normal. That’s dangerous. If your CGM shows you’re consistently in this zone-especially overnight or after exercise-your provider might reduce your SGLT2i dose. This isn’t common yet, but it’s evidence-based and growing.
For other non-insulin drugs like metformin, GLP-1 agonists, or DPP-4 inhibitors, CGM data helps you understand their real-world impact. If your sugar spikes after meals despite taking metformin, maybe you need to adjust timing or dose. If your GLP-1 is causing frequent lows, maybe your insulin dose is too high. CGM gives you the clarity to fine-tune everything.
Common Mistakes and How to Avoid Them
People love CGMs-but they often misuse them. Here are the top errors:
- Stacking insulin: Taking a correction dose, then seeing a double-up arrow and adding more without checking insulin-on-board. Result? A low 2 hours later. Always check your active insulin before adjusting.
- Overreacting to sensor lag: Your glucose might drop fast after a meal because of delayed insulin action. Don’t assume the arrow means you took too much. Wait 15 minutes and see if it stabilizes.
- Ignoring context: A double-down arrow after exercise? That’s normal. A double-down arrow at 3 a.m. with no activity? That’s a problem. Always consider what you did, ate, or took recently.
- Not verifying the reading: If your sensor just started or you had a signal loss, don’t adjust. Wait for a stable reading.
A 2019 case series in Diabetes Care found that 12% of new CGM users increased their hypoglycemia risk by over-correcting downward trends. That’s why education matters.
How to Learn This Right
Most providers don’t teach this unless you ask. Don’t wait for them to bring it up. Ask for a 20-minute session on trend arrow dosing during your next visit.
Good education includes:
- Understanding your personal insulin action time (when does your rapid-acting insulin peak?)
- Recognizing how your body responds to different arrows over time
- Practicing with real examples: “Your glucose is 160 with a single-up arrow. Your correction factor is 1:50. What do you do?”
YouTube educators like Kerri Sparling and the ADA’s own resources have free tutorials. Dexcom also offers printable reference cards through their provider portal. Use them. Tape one to your fridge.
What’s Next? AI and Automated Adjustments
The future is here. In May 2023, the FDA cleared the first app-DAFNE+-that automatically applies the Endocrine Society rules using Dexcom G6 data. It calculates your dose and suggests adjustments without you doing math. In trials, it cut user error by 62%.
Verily’s Onduo platform uses machine learning to predict trends beyond the arrows. In a 2022 NEJM pilot, it reduced hypoglycemia by 38% by spotting patterns humans miss-like a slow rise after stress or a drop after a nap.
But even with AI, you still need to understand the basics. Automation helps. It doesn’t replace knowledge. If you don’t know why your insulin was lowered, you won’t know when to override it.
Final Thought: CGM Is a Tool, Not a Crutch
CGM trend arrows give you superpowers-but only if you use them right. They don’t make you immune to lows or highs. They just give you a better map. The goal isn’t to be perfect. It’s to be proactive. To catch problems before they happen. To spend more time in range, not just reacting to numbers.
If you’re on insulin-or even on SGLT2 inhibitors-this isn’t optional anymore. It’s standard care. The data is clear. The guidelines are solid. The tools are available. The only thing left is to act on it.
Can I use CGM trend arrows to adjust my metformin or GLP-1 dose?
Metformin and GLP-1 agonists don’t cause hypoglycemia on their own, so you don’t adjust them based on CGM arrows like you do with insulin. But CGM data can show you how well they’re working. If your glucose keeps spiking after meals despite taking your GLP-1, you or your provider might consider increasing the dose. If you’re having frequent lows after starting metformin, it could mean your insulin dose is too high, not that metformin is the issue. CGM helps you understand the full picture.
What if my CGM shows a double-down arrow but I feel fine?
You should still take it seriously. CGMs detect glucose changes before symptoms appear. Feeling fine doesn’t mean your glucose isn’t dropping. Especially at night, hypoglycemia can happen without warning. If you see a double-down arrow, reduce your next insulin dose or have a small snack if you’re not planning to eat soon. Don’t wait until you feel shaky.
Do I need to adjust my dose every time I see an arrow?
No. Only adjust for pre-meal boluses or correction doses given more than 3 hours after eating. Don’t adjust for a rising arrow right after a meal-you’re already covered by your carb bolus. Also, if your glucose is already in range and stable, no adjustment is needed. Use the arrows to fine-tune, not to obsess over every small change.
Can I use these guidelines with FreeStyle Libre or other CGMs?
Yes. The Endocrine Society guidelines were based on Dexcom G5, but the principles apply to all CGMs. Abbott’s Libre and Medtronic systems show similar trend arrows. The only difference is the exact speed thresholds for double vs. single arrows. For Libre, double arrows usually mean >3 mg/dL/min, while Dexcom uses >2 mg/dL/min. Adjust your units accordingly based on your personal response. If unsure, start with half the recommended adjustment and check your results over a few days.
What if my provider doesn’t know about these guidelines?
Bring the info. Print out the ADA’s 2023 Standards of Care (Section 7) or the Endocrine Society’s 2017 paper. Many providers haven’t been trained on this, even though it’s standard of care. You’re not asking for a new treatment-you’re asking for the standard one. If they’re hesitant, ask for a referral to a certified diabetes care and education specialist (CDCES). They’re trained in this exact method.





15 Comments