When a critical medication expires, it’s not just a paperwork issue-it’s a patient safety emergency. Imagine a ventilated ICU patient who needs fentanyl for pain and sedation, and the vial on the shelf is dated last month. The nurse pulls it, sees the expiration, and freezes. What now? Swapping in another drug isn’t as simple as grabbing the next one on the shelf. Get it wrong, and you risk withdrawal, respiratory depression, or even death. This isn’t hypothetical. In 2024, over 42% of critical care medications were involved in shortages or expiration events that forced last-minute substitutions. The difference between a smooth transition and a medical error comes down to one thing: having a clear, step-by-step system to prioritize replacements.
Why Expired Medications Are Different From Shortages
Many hospitals treat expired drugs the same way they handle shortages. They’re not the same. A shortage means the drug isn’t being made or shipped. An expired drug is sitting right in front of you-just unusable. That changes everything. You don’t need to wait for a distributor. You don’t need to plead with a vendor. You need to act, fast, with full clinical awareness. The stakes are highest in the ICU. Patients there often need multiple high-risk medications at once: sedatives, vasopressors, neuromuscular blockers, antibiotics. One wrong substitution can cascade into organ failure. A 2023 study of 10,000 ICU patients found that medication errors due to expired or unavailable drugs contributed to 18.7% higher mortality. That’s not a statistic-it’s a team of nurses, pharmacists, and doctors losing a patient because no one had a plan.The Three-Tier Replacement System (ASHP Framework)
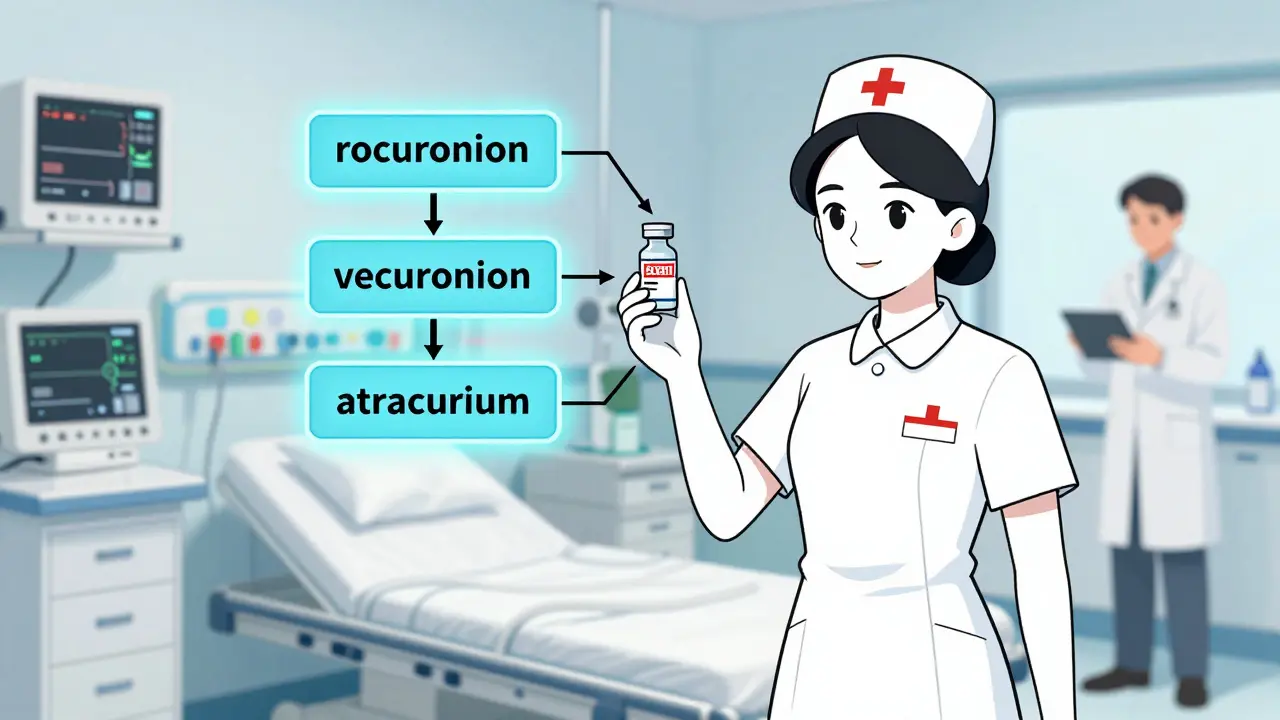
The American Society of Health-System Pharmacists (ASHP) created a proven method for prioritizing alternatives. It’s called the three-tier system. It’s not a suggestion. It’s a standard. Here’s how it works:- 1st Line: The best, most evidence-backed alternative. Same mechanism, similar half-life, same monitoring needs. For example, if cisatracurium expires, rocuronium is the 1st-line substitute for neuromuscular blockade.
- 2nd Line: A good option, but with known differences. Maybe it’s longer acting. Maybe it needs more frequent monitoring. Vecuronium fits here for the same class of drugs.
- 3rd Line: The fallback. Higher risk, more side effects, less predictable. Atracurium or pancuronium fall here. Only use if 1st and 2nd aren’t available.
Step-by-Step: What to Do When a Critical Med Expires
Here’s the exact process used by top-performing ICUs:- Confirm the expiration. Double-check the lot number, date, and storage conditions. Was it stored correctly? Sometimes a drug looks expired but is still stable. Don’t assume-verify.
- Count remaining stock. How many doses are left? Is it just one vial, or 20? If it’s one, you need to act immediately. If it’s 15, you have a few hours to plan.
- Identify affected patients. Who’s on this med right now? Check the electronic record. Are they ventilated? On vasopressors? In renal failure? Each patient’s needs change the best alternative.
- Call the pharmacist. Not the pharmacy tech. The clinical pharmacist. They know the tiers, the dose conversions, and the risks. If your hospital doesn’t have one on-site 24/7, you’re already behind.
- Apply the tiered alternative. Don’t pick the cheapest or the most available. Pick the safest based on the patient’s condition. For example: if fentanyl expires, hydromorphone might be the 1st-line substitute-but only if the patient isn’t renal impaired.
- Update the order set. Change the EHR order. Flag the substitution. Add monitoring parameters (like RASS scores for sedation changes).
- Monitor and document. Watch for signs of under- or over-treatment. Document the reason for the change. This protects the team and helps future decisions.
What Happens When You Don’t Have a Pharmacist
In 68% of community hospitals, there’s no full-time critical care pharmacist. That’s not a typo. That’s the reality for millions of patients. In these settings, replacements are often made by nurses or physicians who aren’t trained in pharmacokinetics. The results? A 2024 survey found that hospitals without pharmacists saw 11.2 more days of hospital stay per medication-related complication. Without expert guidance, common mistakes happen:- Switching from fentanyl to morphine without adjusting for renal clearance-leading to toxicity.
- Using midazolam instead of propofol for sedation, causing prolonged wake-up times.
- Substituting dopamine for norepinephrine in septic shock-increasing arrhythmia risk.
Technology That’s Making a Difference
The best hospitals aren’t just using paper lists anymore. They’re using tech:- Automated expiration alerts: Systems that flag drugs with 30 days or less until expiry. 68% of hospitals with under 5% expired meds use this.
- Bar-code scanning with substitution prompts: When a nurse scans an expired drug, the system pops up the approved alternative with dose guidance.
- AI-driven substitution tools: Pilot systems at CU Anschutz analyze 147 patient factors-age, kidney function, liver status, current meds-and recommend the safest alternative. Early results show 94.7% agreement with expert pharmacists.
The Human Factor: Why Culture Matters
Even the best system fails without the right culture. In hospitals with strong protocols, teams meet daily to review meds. Pharmacists sit with doctors at the bedside. Nurses speak up when something feels off. In contrast, at hospitals without this culture, staff say things like:- “We just used what we had.”
- “The doctor said it was fine.”
- “We didn’t have time.”
What’s Changing in 2025 and Beyond
The FDA is moving toward longer expiration dates based on real stability data-not arbitrary labels. A new draft guideline could cut unnecessary waste by 20%. ASHP is finalizing new guidelines in early 2026 that will treat expired meds as a separate category from shortages. But the biggest shift? The recognition that pharmacists aren’t just dispensers-they’re clinical decision-makers. A 2025 study in Pharmacotherapy called pharmacist-led medication management “a standard of care, not an option.” The future belongs to hospitals that treat medication safety like infection control: non-negotiable, system-driven, and staffed by experts.What You Can Do Today
You don’t need a big budget or a tech upgrade to start. Here’s what you can do right now:- Ask your pharmacy: “Do we have a written, tiered replacement list for our top 10 critical meds?”
- If not, make one. Start with fentanyl, norepinephrine, propofol, cisatracurium, and vancomycin.
- Print it. Put it on the wall. Train every nurse and resident on it.
- Assign one pharmacist to own this process. No exceptions.
- Set up a 30-day expiration alert in your inventory system-even if it’s a simple spreadsheet.
What’s the most common mistake when replacing expired critical medications?
The most common mistake is assuming all drugs in the same class are interchangeable. For example, switching from fentanyl to morphine without adjusting the dose for kidney function can cause fatal respiratory depression. Each drug has unique pharmacokinetics-half-life, metabolism, active metabolites. You can’t swap them like light bulbs.
Can expired medications ever be used if they’re just a day past the date?
No. The expiration date is a legally binding guarantee of potency and safety. Even one day past it, the drug may have degraded. In critical care, where precision matters, you cannot risk reduced efficacy or toxic byproducts. Always discard expired meds-no exceptions.
Why can’t we just order more of the same drug instead of switching?
Because the supply chain doesn’t work that fast. Even with emergency orders, delivery can take 24-72 hours. In the ICU, patients need meds every hour. Waiting isn’t an option. That’s why having pre-approved alternatives is critical. You can’t rely on delivery when someone’s on a ventilator.
Do community hospitals have the same resources as big hospitals for handling expired meds?
No. Only 42% of community hospitals have formal replacement protocols, compared to 89% of academic centers. Many lack 24/7 pharmacists, automated alerts, or EHR integration. This creates a dangerous gap in care. Patients in small hospitals are more likely to get suboptimal or unsafe substitutions.
Is there a list of approved alternatives for common critical meds?
Yes. The ASHP Guidelines and the FDA Drug Shortages Database include tiered alternatives for over 150 critical medications. These are publicly available and should be downloaded, reviewed, and adapted by every hospital. Don’t guess-use the evidence.
How often should replacement protocols be reviewed?
At least every six months-or anytime a new drug is added to the formulary or a major shortage occurs. Drug interactions, dosing guidelines, and availability change constantly. A protocol from 2022 may be outdated or unsafe today.