Most people don’t realize how much sodium is hiding in their food. You might think cutting back on the salt shaker is enough, but that’s only a small part of the story. In fact, sodium in processed and restaurant meals makes up 70% or more of what we consume daily. And for people with high blood pressure, that’s a major problem.
High sodium intake doesn’t just raise your blood pressure-it makes your heart work harder, stiffens your arteries, and can undo the effects of your blood pressure meds. The good news? Cutting back on sodium doesn’t require extreme changes. Even small, consistent shifts can lower your systolic blood pressure by 5 to 8 mm Hg in just a few weeks. And you don’t have to go cold turkey to see results.
Why Sodium Raises Blood Pressure
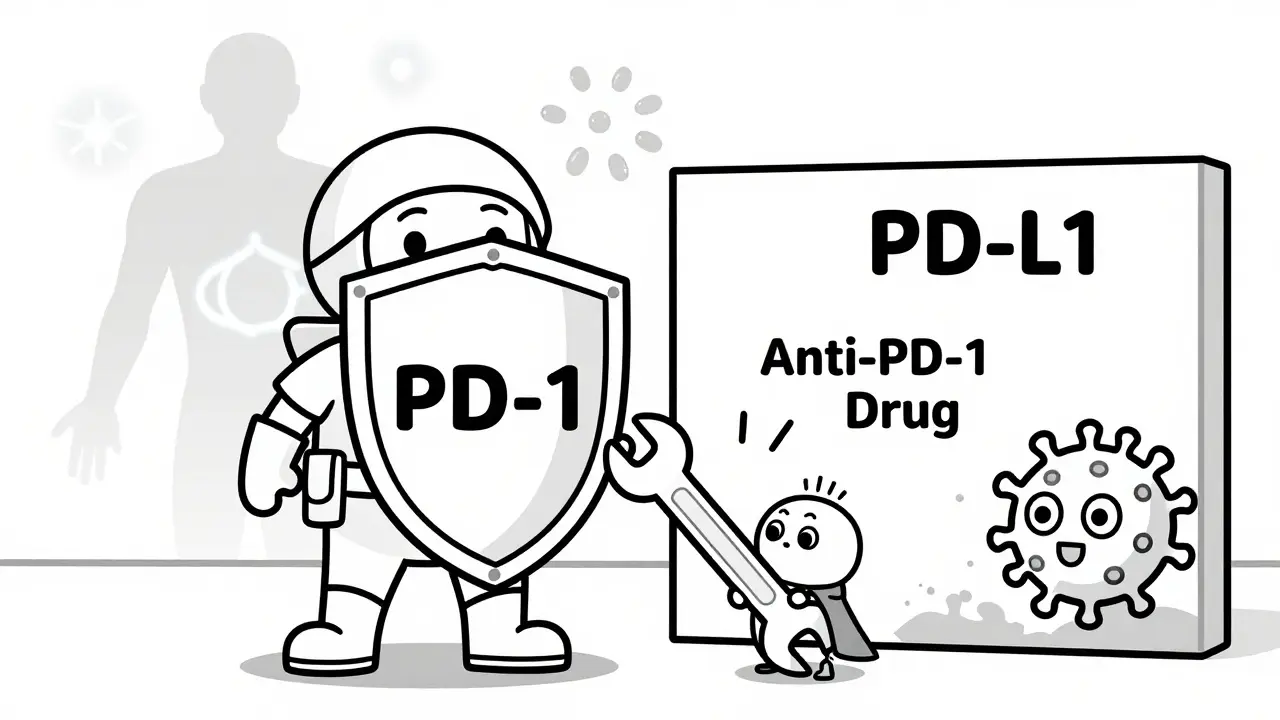
Your body needs a little sodium to function-nerve signals, muscle contractions, fluid balance. But too much? It turns into a problem fast. When you eat excess sodium, your kidneys hold onto more water to dilute it. That extra fluid increases blood volume, which pushes harder against your artery walls. Over time, that pressure damages your blood vessels and forces your heart to pump harder.
It’s not just about volume, though. High sodium also messes with your blood vessel lining. It reduces nitric oxide, a natural chemical that helps arteries relax. Without enough of it, your vessels stay tight, increasing resistance and pushing blood pressure even higher. Studies show that people with hypertension experience a stronger reaction-up to 5.4 mm Hg drop in systolic pressure when they cut sodium by 1.75 grams per day.
And here’s the kicker: about half of people with high blood pressure are “salt sensitive.” That means their blood pressure reacts sharply to sodium changes. Even if you don’t know you’re salt sensitive, reducing sodium is still one of the safest, most effective things you can do.
What the Experts Say About Sodium Limits
The American Heart Association says the ideal daily sodium limit is 1,500 mg. The World Health Organization says no more than 2,000 mg. The maximum most guidelines accept is 2,300 mg-about a teaspoon of salt. But the average American eats over 3,400 mg a day. That’s nearly 50% more than the upper limit.
Here’s what matters: you don’t have to hit 1,500 mg right away. Even dropping from 3,400 mg to 2,500 mg can lower your blood pressure. The CARDIA-SSBP study found that after just one week on a low-sodium diet, participants saw an average 8 mm Hg drop in systolic pressure. That’s as effective as starting a first-line blood pressure medication.
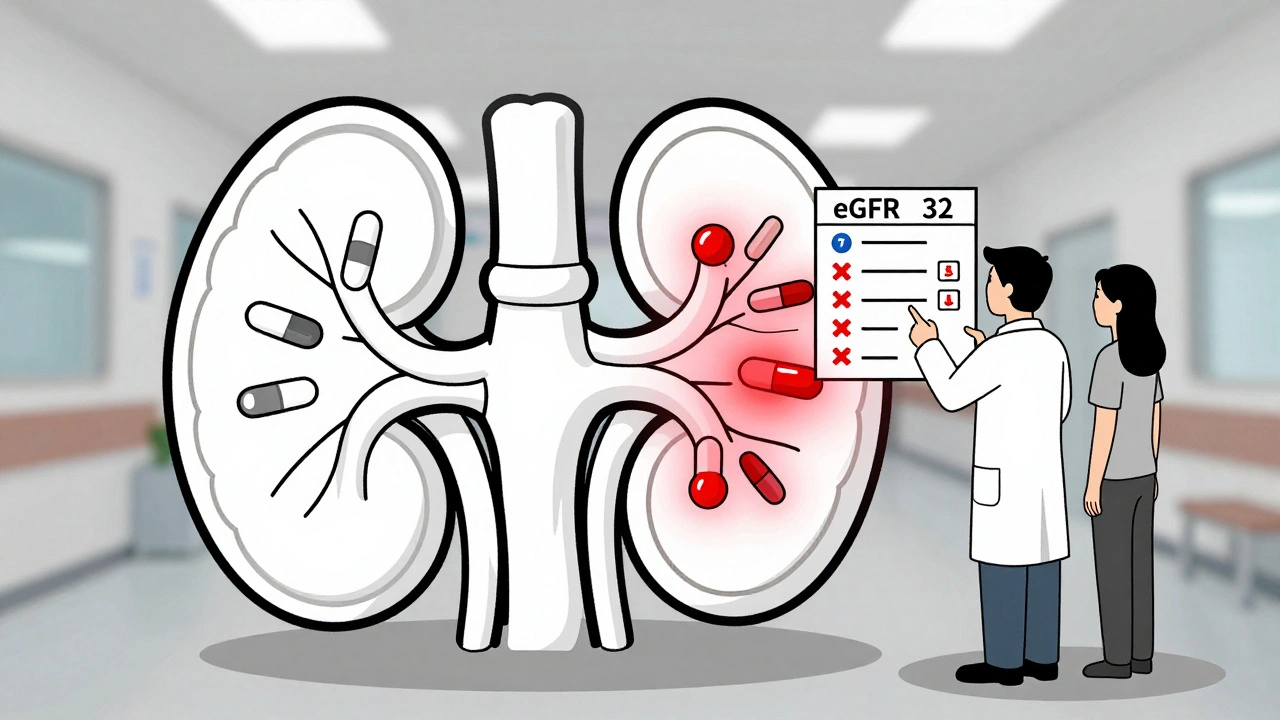
But there’s a twist. Some research suggests that going too low-below 1,500 mg-might not help everyone. A few people, especially those with advanced heart or kidney disease, can actually see negative effects. That’s why most experts recommend aiming for the 1,500-2,300 mg range, not chasing the lowest number possible.
Where the Sodium Is Really Hiding
It’s not the salt you add at the table. It’s not even the salt you sprinkle while cooking. The real culprits are packaged and restaurant foods.
- A single fast-food burger can have 1,500 mg of sodium.
- A bowl of canned soup? Often 800-1,200 mg.
- Two slices of store-bought bread? Around 400 mg.
- A “healthy” salad with bottled dressing and croutons? Up to 1,200 mg.
Even foods you think are low-sodium aren’t. Yogurt, cheese, frozen meals, deli meats, and condiments like soy sauce and ketchup are loaded. One tablespoon of soy sauce has 1,000 mg. That’s almost half your daily limit in one spoonful.
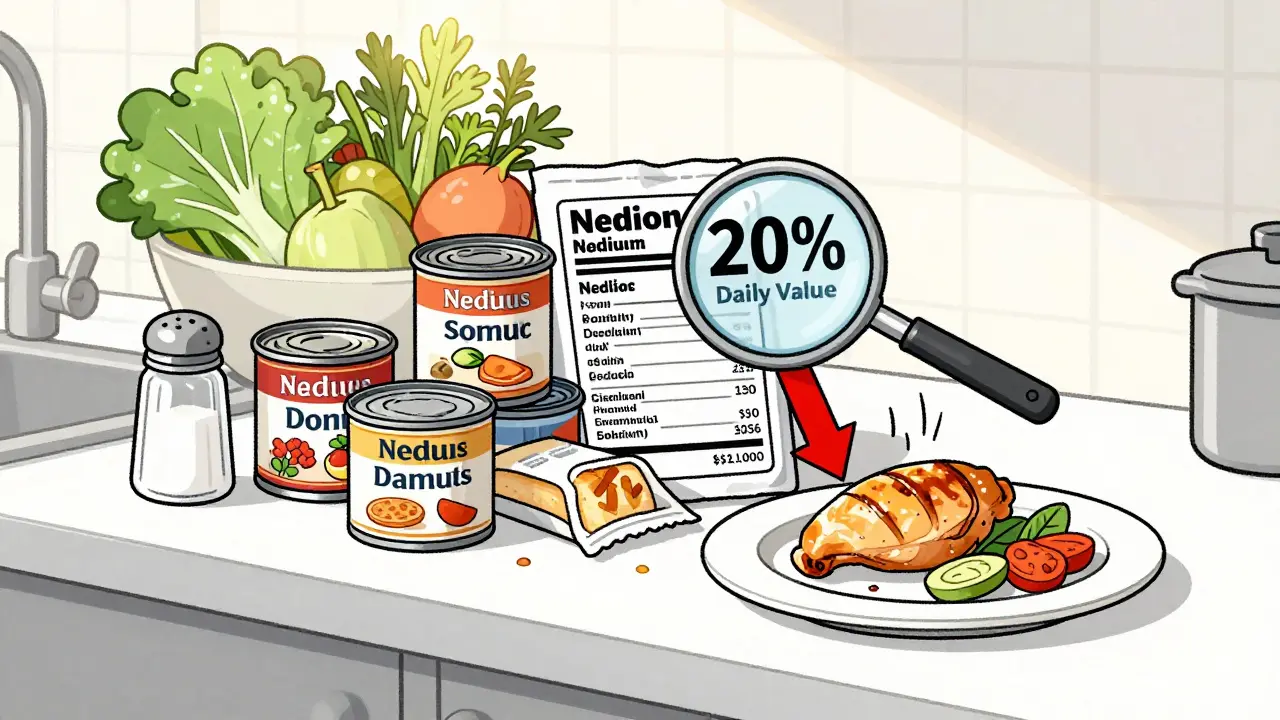
That’s why reading labels is non-negotiable. The FDA now requires sodium content to be bolded on nutrition labels. Look for “% Daily Value.” Anything over 20% per serving is high. Aim for under 5% if you’re trying to cut back.

5 Practical Ways to Reduce Sodium Right Now
Changing your diet doesn’t mean giving up flavor. It means learning new ways to get taste without salt.
- Swap processed for whole foods. Fresh vegetables, fruits, lean meats, beans, and plain grains have almost no sodium. Cook them yourself. A home-cooked chicken and veggie stir-fry can have 400 mg of sodium. The same dish from a restaurant? Often over 1,800 mg.
- Use herbs, spices, and acids. Garlic, onion powder, black pepper, cumin, paprika, and chili flakes add depth. Lemon juice, vinegar, and lime zest brighten flavor without salt. One study found that people who used citrus and herbs reduced their salt use by 30-50% without noticing a drop in satisfaction.
- Choose low-sodium versions. Look for “no salt added,” “low sodium,” or “unsalted” on labels. Low-sodium broth can cut 500 mg per cup. But be careful-some “low-sodium” products replace salt with potassium chloride, which isn’t safe for everyone (especially those with kidney issues).
- Go easy on condiments. Skip the soy sauce, teriyaki, and bottled salad dressings. Make your own vinaigrette with olive oil, vinegar, and mustard. Use mustard instead of mayo on sandwiches. A teaspoon of regular mayo has 75 mg sodium; the low-fat version? Often over 100 mg.
- Ask for it on the side at restaurants. Request sauces, dressings, and seasonings separately. You can control how much you use. Choose grilled, steamed, or roasted over fried. Skip the bread basket and salty appetizers.
The DASH Diet: Proven to Lower Blood Pressure
The DASH diet (Dietary Approaches to Stop Hypertension) isn’t a fad. It’s a science-backed eating plan developed by the National Heart, Lung, and Blood Institute. It focuses on vegetables, fruits, whole grains, lean proteins, and low-fat dairy-all while limiting sodium, saturated fat, and added sugar.
When combined with sodium reduction under 2,300 mg per day, DASH lowers systolic blood pressure by 8-14 mm Hg. That’s more than most medications. The 2022 OmniHeart Trial showed that replacing some carbs with protein or healthy fats in a DASH-style diet made blood pressure drop even further.
You don’t need to follow DASH perfectly. Start by adding one extra serving of vegetables a day, swapping white rice for brown, and choosing yogurt over cheese. Small steps add up.
What About Salt Substitutes?
Products like Mrs. Dash, NoSalt, or LoSalt replace sodium chloride with potassium chloride. They can cut 300-500 mg of sodium per meal. That’s a big help.
But they’re not for everyone. If you have kidney disease, heart failure, or take certain blood pressure meds (like ACE inhibitors or potassium-sparing diuretics), extra potassium can be dangerous. Always check with your doctor before switching to a salt substitute.
For most healthy people, though, potassium is a bonus. The body needs 3,500-5,000 mg daily, but most people get less than half that. Potassium helps your kidneys flush out sodium and relaxes blood vessel walls. Bananas, spinach, sweet potatoes, beans, and avocados are great sources.

Real People, Real Results
On Reddit’s r/HighBloodPressure community, users share stories of taste adaptation. One person wrote: “It took three weeks for my taste buds to reset. Now, my old favorite pizza tastes like a salt bomb.” Another said they started using smoked paprika and apple cider vinegar-and stopped craving salt entirely.
Those who used the American Heart Association’s “Sodium Swap” app for 30 days saw an average 6.3 mm Hg drop in systolic pressure. The key? Tracking. Writing down what you eat makes you aware of hidden sodium. You start noticing patterns: “Oh, I always add salt to my oatmeal. Why?”
Cost is a concern. Fresh food often costs more than processed. But batch-cooking on weekends saves time and money. A big pot of low-sodium chili, roasted veggies, and brown rice can last all week. It’s cheaper than takeout and far healthier.
What If Your Blood Pressure Doesn’t Drop?
Most people see results. But about 5% of individuals experience what’s called “inverse salt sensitivity”-their blood pressure actually rises when they cut sodium. This is rare, but real. It can happen if someone has undiagnosed hormonal imbalances, severe kidney issues, or isn’t following the diet correctly.
If you’ve cut sodium for 6-8 weeks and your blood pressure hasn’t budged, talk to your doctor. You might need to check for other contributors: sleep apnea, high stress, low potassium, or medication interactions. Sodium isn’t the only factor-but it’s one of the most controllable.
Start Small. Stay Consistent.
You don’t need to overhaul your life overnight. Pick one thing: swap your soup for low-sodium broth. Skip the soy sauce on your stir-fry. Buy plain yogurt and add your own fruit. That’s enough to start.
Within two weeks, you’ll notice food tastes different. Not bland-just more real. You’ll taste the sweetness in tomatoes, the earthiness in mushrooms, the tang in vinegar. Your palate resets. And your blood pressure starts to follow.
Lowering sodium isn’t about perfection. It’s about progress. Every 1,000 mg you cut per day reduces your stroke risk by 8% and heart disease risk by 6% over 10 years. That’s not a miracle. That’s math. And it’s within your control.





10 Comments