Supplement-Drug Interaction Checker
Enter your medications and supplements below to check for potential dangerous interactions. Note: This tool uses a limited database based on FDA reports and medical literature. Always consult your pharmacist or doctor for personalized medical advice.
Every year, millions of people in the U.S. take supplements alongside prescription drugs-vitamins, herbs, protein powders, sleep aids, and more. But here’s the problem: supplement labels rarely tell you if those pills could clash dangerously with your medications. Unlike prescription drugs, which come with clear, legally required warnings, supplements are mostly left to their own devices. That means you’re on your own to figure out if that turmeric capsule could interfere with your blood thinner, or if your magnesium supplement might mess with your thyroid medicine.
What’s Actually on a Supplement Label?
If you’ve ever looked at a supplement bottle, you’ve seen the Supplement Facts panel. It looks a lot like a nutrition label. It lists the serving size, how much of each ingredient is in one serving, and sometimes a % Daily Value. But here’s what’s missing: drug interaction warnings.The FDA doesn’t require supplement makers to test for interactions with medications. That’s not a mistake-it’s the law. Under the Dietary Supplement Health and Education Act (DSHEA) of 1994, supplements are treated like food, not drugs. That means manufacturers don’t need FDA approval before selling them. They don’t need to prove safety. They don’t need to prove effectiveness. And they don’t need to warn you about risks when taken with your pills.
So what’s actually on the label? The ingredient list. But watch out for proprietary blends. These are groups of ingredients listed together without individual amounts. For example: "Energy Blend: 500mg (green tea extract, caffeine, L-theanine)." You don’t know how much of each is in there. One brand’s "Energy Blend" might have 200mg of caffeine. Another’s might have 400mg. That’s the difference between a mild boost and a heart-racing panic attack-especially if you’re on a beta-blocker or antidepressant.
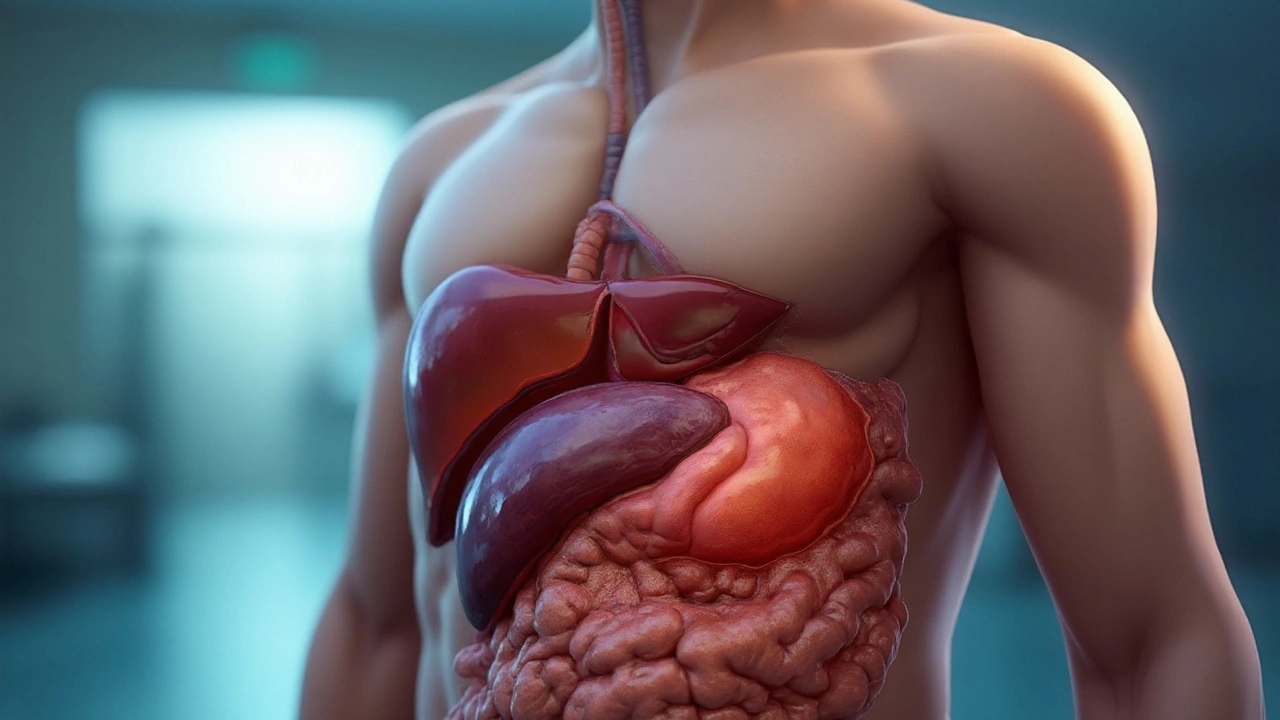
Also check the other ingredients list. That’s where allergens like soy, milk, or shellfish must be disclosed. But it doesn’t tell you about inactive ingredients that might affect how your body absorbs your medication. For example, some calcium supplements use magnesium stearate as a filler. While generally safe, it can slow absorption of certain antibiotics like tetracycline.
How Drug Labels Work (And Why They’re Different)
Prescription and over-the-counter (OTC) drug labels follow strict rules. They use the Drug Facts format with clear sections: Active Ingredients, Purpose, Uses, Warnings, Directions, and Inactive Ingredients.The Warnings section is where the real safety info lives. It tells you:
- When not to take the drug (e.g., "Do not use if you have liver disease")
- When to call your doctor (e.g., "If you experience dizziness or blurred vision")
- What drugs to avoid (e.g., "Do not take with warfarin or aspirin")
According to FDA data, 97% of prescription drugs and 89% of OTC drugs include specific interaction warnings. That’s because drug makers are required to run clinical studies proving how their product interacts with other medications. Supplement makers? Not even close.
A 2021 FDA review of 500 popular supplements found that only 12.7% included any drug interaction warning. That’s not a typo. That’s the system.
Real-World Interactions You Can’t Afford to Ignore
Here are five dangerous combinations you might not know about:- Warfarin + Vitamin K: Warfarin (Coumadin) is a blood thinner. Vitamin K helps your blood clot. If you take green tea extract, spirulina, or a multivitamin with high vitamin K, it can make warfarin less effective. Studies show this can reduce warfarin’s effect by 30-50%, increasing your risk of stroke or clot.
- St. John’s Wort + Digoxin: This herbal remedy for depression can drop digoxin (used for heart failure) levels in your blood by 26%. That means your heart condition could worsen without you knowing.
- CoQ10 + Warfarin: Many people take CoQ10 for heart health or statin side effects. But it can shorten your prothrombin time by 15-25%, making warfarin less effective. This isn’t theory-it’s documented in FDA safety reports.
- Metformin + Milk Thistle: People with diabetes sometimes take milk thistle to "protect the liver." But it can boost metformin’s effect, causing dangerous low blood sugar. One patient reported a blood glucose level of 42 mg/dL after adding milk thistle-well below the danger zone of 70.
- Antiretrovirals + High-Dose Vitamin C: If you’re on HIV meds, taking more than 1,000 mg of vitamin C daily can lower drug levels by 22% by changing stomach pH. That means the virus could start replicating again.
These aren’t rare cases. The FDA recorded 1,960 supplement-related adverse events in 2022. Nearly 28% involved possible drug interactions. And those are just the ones reported.
How to Protect Yourself: A Practical Guide
You can’t rely on the label. So here’s what you actually need to do:- Take a photo of every supplement bottle. Keep them in your phone gallery. When you see your doctor or pharmacist, show them-not just tell them. Many people forget what they’re taking after a few weeks.
- Use a free interaction checker. Go to Medscape’s Drug Interaction Checker. It’s free, no login needed, and checks over 24,000 drug pairs. Type in your prescription and your supplement. It will tell you if it’s a major, moderate, or minor interaction.
- Ask your pharmacist. Not your doctor. Pharmacists are the drug experts. They see hundreds of interactions every week. Ask: "I’m taking [medication]. Is it safe to take [supplement]?" Don’t say "I think it’s natural, so it’s fine."
- Check for USP verification. The USP (U.S. Pharmacopeia) seal means the product was independently tested for purity, potency, and accurate labeling. Only 18% of supplements have it. But those that do are far more reliable. Look for the "USP Verified" mark on the bottle.
- Assume "natural" doesn’t mean safe. Red yeast rice contains monacolin K-the same active ingredient as the prescription statin lovastatin. Taking it with another statin? You’re doubling your dose. That can cause muscle damage or kidney failure.
Why This System Is Broken-and What’s Changing
The supplement industry made $53.1 billion in 2023. Yet the FDA’s entire Office of Dietary Supplement Programs has a $4.7 million budget. That’s less than 0.03% of the FDA’s total spending. They inspect a tiny fraction of products. Most recalls happen only after someone gets hurt.In March 2024, the FDA released a draft guidance suggesting supplement labels voluntarily add interaction warnings. But without a law, most companies won’t bother. Congress tried to fix this in 2022 with the Dietary Supplement Listing Act. It failed by two votes.
But change is coming slowly. The American Medical Association now recommends doctors spend 3-5 minutes during annual checkups asking patients about supplements. Johns Hopkins estimates this could prevent 28,000 ER visits a year.
The FDA is also testing QR codes on supplement labels. Scan the code, and you get a real-time interaction report. It’s still in pilot mode, but it’s the first real step toward closing the gap.

What to Do Right Now
You don’t need to stop taking supplements. But you need to take control.- Stop guessing. Start checking.
- Don’t assume your doctor knows what you’re taking. They rarely ask.
- Don’t trust "all-natural" claims. They mean nothing legally.
- When in doubt, pause. Wait. Ask.
If you’re on blood thinners, thyroid meds, diabetes drugs, antidepressants, or heart medications-your supplement could be silently undermining your treatment. You don’t need to be a scientist to protect yourself. You just need to be informed.
Do supplement labels have to warn about drug interactions?
No. Under current U.S. law (DSHEA), supplement manufacturers are not required to include drug interaction warnings on their labels. Only prescription and over-the-counter drugs must list these warnings. Most supplement labels don’t mention interactions at all-only about 13% do voluntarily.
Can I trust the "natural" label on supplements?
No. "Natural" has no legal meaning in supplement labeling. It doesn’t mean safer, more effective, or free of interactions. Red yeast rice, for example, is natural-and it contains the same active ingredient as the prescription statin lovastatin. Taking it with another statin can cause dangerous muscle damage.
What should I do if my supplement doesn’t list any warnings?
Don’t assume it’s safe. Always check with your pharmacist or use a trusted drug interaction tool like Medscape’s free checker. Take a photo of the label and bring it to your doctor. Many people assume no warning means no risk-but the truth is, the warning isn’t required by law.
Are all supplements dangerous with medications?
No. Many supplements are safe when used properly. But the risk is unpredictable because there’s no standard testing. The danger isn’t the supplement itself-it’s the lack of information. A vitamin D pill is usually fine. But if you’re on a steroid, it could affect calcium levels. The only way to know is to check each combination individually.
What’s the best way to tell if a supplement is high quality?
Look for the USP Verified mark. This means an independent lab tested the product for accurate ingredient amounts, purity, and lack of contaminants. Only about 18% of supplements have this certification. Products without it may contain less of the active ingredient than listed-or even harmful contaminants like heavy metals.
Should I stop taking supplements if I’m on medication?
Not necessarily. But you should never start or keep taking one without checking for interactions. Many supplements-like vitamin D, magnesium, or omega-3s-can be safe and even helpful. But you need to confirm it with your pharmacist. Don’t rely on the label. Don’t rely on Google. Talk to a professional.
Final Thought: You’re the Last Line of Defense
The system isn’t designed to protect you. The FDA doesn’t have the resources. The supplement industry doesn’t have the incentive. Your doctor might not ask. So the responsibility falls to you. Read the label. Check the ingredients. Use a reliable tool. Ask the pharmacist. Take a photo. Keep a list.It’s not about fear. It’s about control. You’re already taking supplements because you want to feel better. Don’t let a hidden interaction undo all that work.






8 Comments