Many older adults take medications like oxybutynin for overactive bladder, diphenhydramine for allergies, or amitriptyline for nerve pain without realizing they’re on drugs that can quietly damage their brain. These are anticholinergics-a class of medications that block acetylcholine, a key chemical in the brain and body. They work well for their intended purposes, but the hidden cost? Memory loss, brain shrinkage, and constant dry mouth. And for many, the risks aren’t just theoretical-they’re happening right now.
What Anticholinergics Do to Your Brain
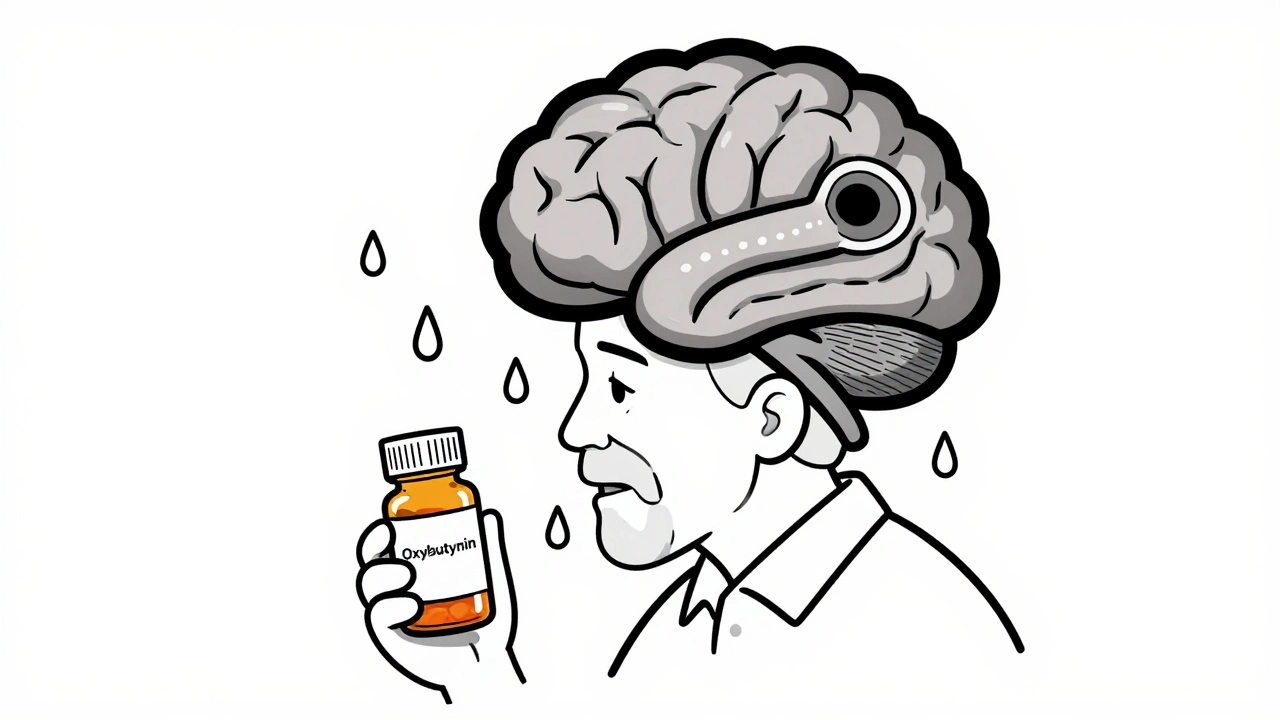
Anticholinergics don’t just stop your bladder from spasming or your nose from running. They interfere with how your brain remembers things, makes decisions, and stays sharp. Every time you take a high-dose anticholinergic, you’re reducing the flow of acetylcholine in areas like the hippocampus and prefrontal cortex-regions critical for memory and attention. Studies using brain scans show that people on these drugs lose brain volume faster. One major study of 451 older adults found that those on medications with high anticholinergic burden (ACB score of 2 or 3) lost 0.5% to 1.2% more brain tissue each year than those not taking them. That’s not a small difference-it’s the kind of change you see in early Alzheimer’s. Glucose metabolism in the hippocampus dropped by 8-14%, meaning those brain cells weren’t getting enough fuel to work properly. Ventricles-the fluid-filled spaces in the brain-grew 10-15% larger, a sign of tissue loss. Cognitive tests confirmed the damage. People on these drugs scored 23-32% worse on memory recall tasks and 18-27% worse on problem-solving tests. The worse the score on the ACB scale, the worse the decline. Each extra point on the scale meant an additional 0.3% brain shrinkage per year. It’s dose-dependent, time-dependent, and cumulative. Three years of use? That doubles your risk of dementia, according to a study of over 48,000 people published in the BMJ.Not All Anticholinergics Are the Same
You might think all anticholinergics are equally risky. They’re not. The difference between drugs can mean the difference between keeping your mind sharp or losing it. Drugs like scopolamine (used for motion sickness) and oxybutynin (for bladder control) have the highest ACB score-3. They cross the blood-brain barrier easily and hit the M1 receptors in the brain hard. Oxybutynin, in particular, causes a 28% greater decline in cognitive scores compared to tolterodine, another bladder drug with a lower ACB score (1-2). A 2020 analysis of 12 clinical trials showed this clearly: oxybutynin users performed significantly worse on memory and attention tests. But here’s the good news: many alternatives exist. Drugs like glycopyrrolate, trospium, tolterodine, darifenacin, and tiotropium all have an ACB score of 1 or lower. Multiple studies, including a 2023 review in PMC, found no significant cognitive decline in users of these medications. Even better, mirabegron (brand name Myrbetriq) works just as well for overactive bladder but has zero anticholinergic activity. It’s a beta-3 agonist, not a cholinergic blocker. In a head-to-head trial published in the New England Journal of Medicine, mirabegron matched oxybutynin’s effectiveness-without the brain fog. So why don’t more doctors switch patients? Cost. Generic oxybutynin costs about $15 a month. Mirabegron runs $350. For many, the price tag outweighs the risk-even when the risk is brain damage.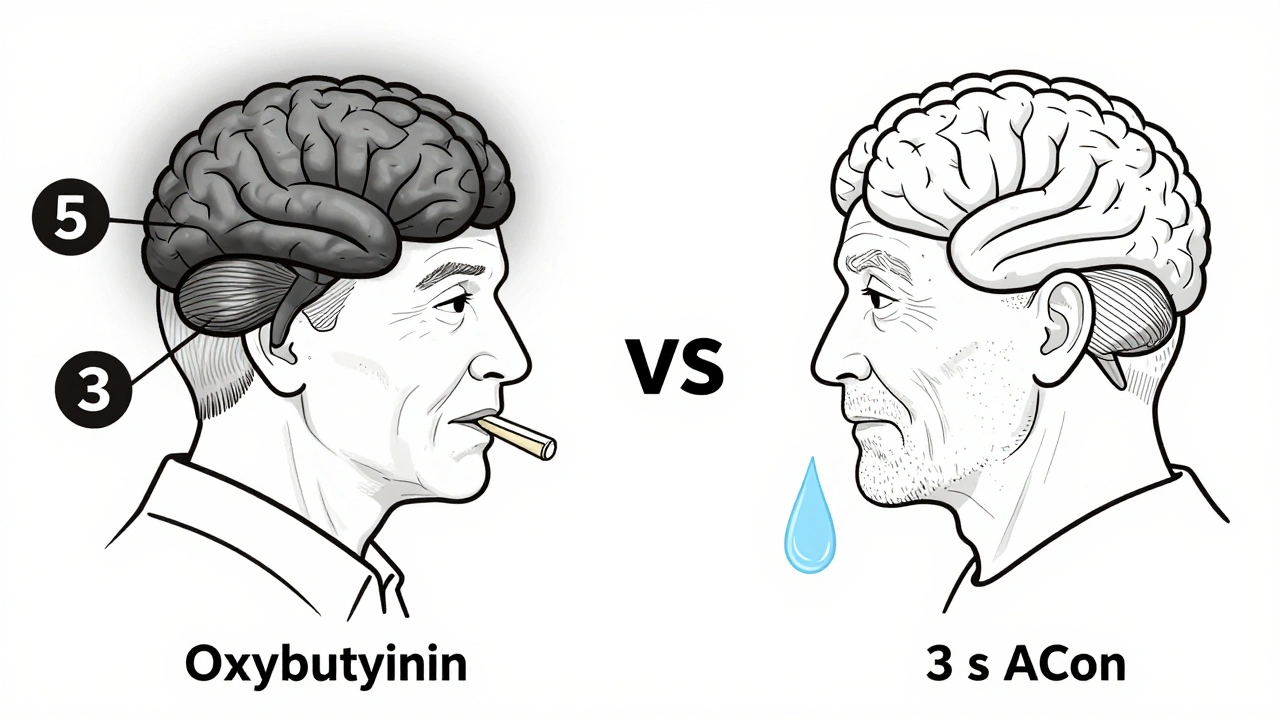
Why Dry Mouth Is More Than Just an Annoyance
Dry mouth is the most common side effect of anticholinergics. Up to 82% of users report it on patient review sites like Drugs.com. But it’s not just uncomfortable-it’s a warning sign. Acetylcholine tells your salivary glands to make saliva. Block it, and your mouth goes dry. People describe it as constant thirst, needing to drink 2-3 liters of water a day. Some can’t speak clearly. Others can’t swallow pills. Eating becomes a chore. And dry mouth isn’t just about comfort-it raises your risk of tooth decay, gum disease, and oral infections. Saliva doesn’t just moisten your mouth; it protects your teeth and fights bacteria. Managing it isn’t hard, but most people don’t know how. Sugar-free gum or lozenges can boost saliva production by 30-40%. Prescription saliva substitutes like Xerolube cost $25-40 a month. For severe cases, pilocarpine (5mg three times daily) can increase saliva flow by 50-70%, as shown in a 2018 NEJM study. But few doctors mention these options. Patients are left to suffer in silence.Who’s at Risk-and Who Should Stop
The American Geriatrics Society says this clearly: avoid anticholinergics in adults 65 and older. Their 2023 Beers Criteria list includes 56 medications as potentially inappropriate for seniors. Top offenders: diphenhydramine (Benadryl), oxybutynin, and amitriptyline. These are often prescribed for things that could be treated differently-like occasional nighttime allergies or mild nerve pain. But it’s not just about age. Anyone taking multiple medications is at higher risk. Polypharmacy is the silent killer here. A 70-year-old on oxybutynin for bladder control, amitriptyline for pain, and diphenhydramine for sleep is on three high-ACB drugs. Their total burden? ACB score of 9. That’s not just risky-it’s dangerous. And the damage isn’t always obvious. On Reddit’s r/agingparents, 78% of 142 respondents reported sudden confusion or memory lapses in relatives after starting oxybutynin. One woman’s MMSE score dropped from 29/30 to 22/30 after five years on amitriptyline. That’s a slide from normal cognition to mild dementia. Still, stopping isn’t always easy. For Parkinson’s patients, anticholinergics like trihexyphenidyl can be essential. Abruptly stopping them can cause tremors, stiffness, and falls. The key isn’t blanket avoidance-it’s smart management.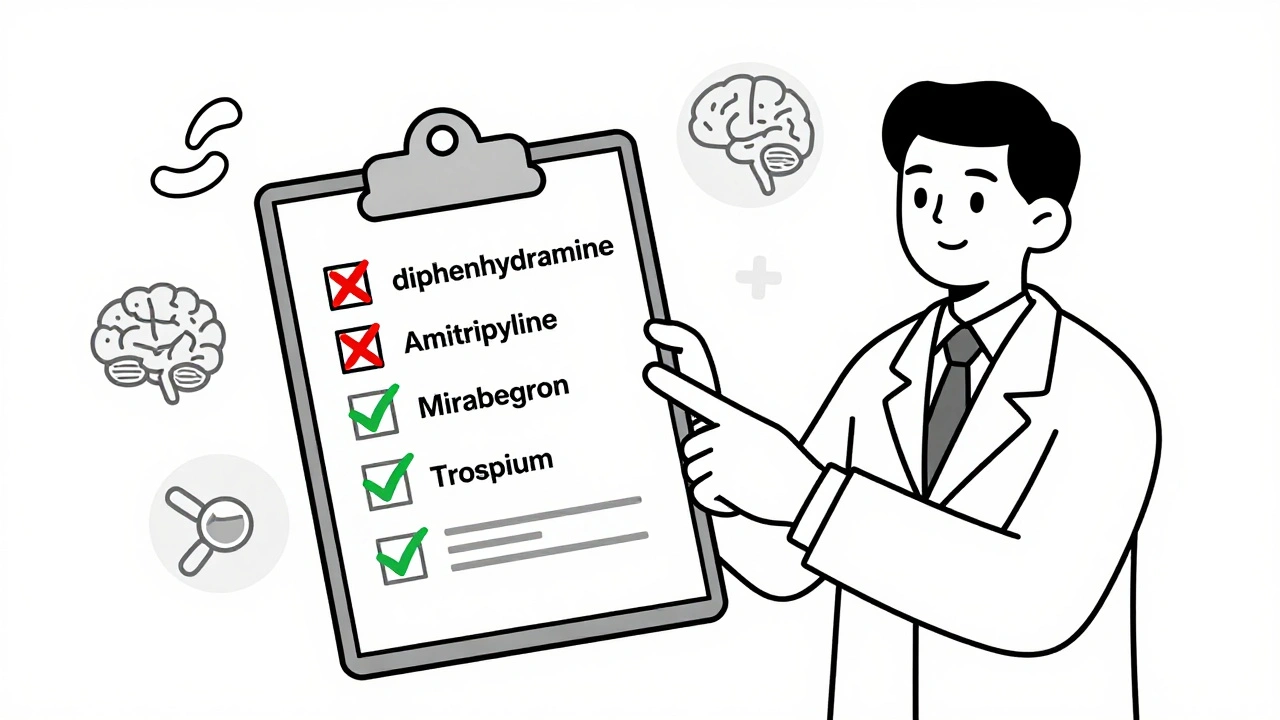
What You Can Do Now
If you or someone you care about is on an anticholinergic, here’s what to do:- Check the ACB score. Look up the drug on the Anticholinergic Cognitive Burden scale. Is it a 2 or 3? If so, ask your doctor about alternatives.
- Ask about mirabegron. For overactive bladder, it’s just as effective as oxybutynin-with no brain risk.
- Review all meds. Look at every pill, even OTC ones. Diphenhydramine is in sleep aids, cold meds, and allergy pills. It’s hiding in plain sight.
- Ask for cognitive testing. Ask your doctor to do a Montreal Cognitive Assessment (MoCA) every six months if you’re on long-term anticholinergics.
- Manage dry mouth. Use sugar-free gum, sip water, and ask about pilocarpine if it’s severe.
The Bigger Picture
The global market for anticholinergics hit $8.7 billion in 2023. That’s billions in sales for drugs that are increasingly linked to brain damage. Yet, prescriptions for high-risk ones like oxybutynin have dropped 32% among Medicare patients since 2015. Why? Because awareness is growing. The FDA updated labels in 2022 to warn about cognitive risks. The UK’s NICE now recommends deprescribing anticholinergics in 68% of long-term users over 65. Newer drugs are coming. Trospium chloride XR (Sanctura XR) has 70% less brain penetration than oxybutynin. Karuna Therapeutics is testing xanomeline, a drug that targets brain receptors without causing dry mouth. AI tools like MedAware are being rolled out to flag risky prescriptions before they’re written. The message is clear: anticholinergics aren’t harmless. They’re powerful tools-but they come with serious, measurable costs. For many, the trade-off isn’t worth it. With safer alternatives available and better screening tools on the horizon, there’s no reason to keep taking them unless there’s no other choice.Can anticholinergics cause permanent brain damage?
Long-term use of high-ACB anticholinergics is linked to accelerated brain shrinkage, reduced brain activity, and increased risk of dementia. While some cognitive decline may improve after stopping the drug, studies show that 63% of long-term users progress to mild cognitive impairment or Alzheimer’s within 10 years. The structural changes seen on MRI-like larger ventricles and lower hippocampal volume-are often irreversible.
Is dry mouth from anticholinergics dangerous?
Yes. Chronic dry mouth increases the risk of tooth decay, gum disease, fungal infections like thrush, and difficulty swallowing or speaking. It can also lead to poor nutrition if eating becomes too uncomfortable. Saliva protects your mouth by neutralizing acids and washing away bacteria. Without it, oral health declines quickly.
What are the safest alternatives to oxybutynin for overactive bladder?
Mirabegron (Myrbetriq) is the most effective alternative-it works just as well as oxybutynin but has no anticholinergic activity. Other options include tolterodine (ACB 1-2), darifenacin (ACB 1), and non-drug approaches like pelvic floor therapy, bladder training, and timed voiding. For many, these are safer long-term choices.
Can I stop taking anticholinergics cold turkey?
No-not without medical supervision. Stopping suddenly can cause rebound symptoms like severe bladder spasms, worsening Parkinson’s tremors, or withdrawal anxiety. Always work with your doctor to taper off slowly. They can help you switch to safer alternatives while managing symptoms.
Are over-the-counter anticholinergics like Benadryl safe?
No, especially for older adults. Diphenhydramine (Benadryl) has an ACB score of 3-the highest risk level. It’s linked to memory problems, confusion, and increased dementia risk. Many people take it nightly for sleep, not realizing it’s a potent brain-altering drug. Safer sleep aids include melatonin or cognitive behavioral therapy for insomnia.







8 Comments