When you’re struggling to breathe, it’s hard to tell if it’s asthma or COPD. Both make you wheeze, cough, and feel out of breath. But they’re not the same condition - and treating them the wrong way can make things worse.
What’s Really Going On in Your Lungs?
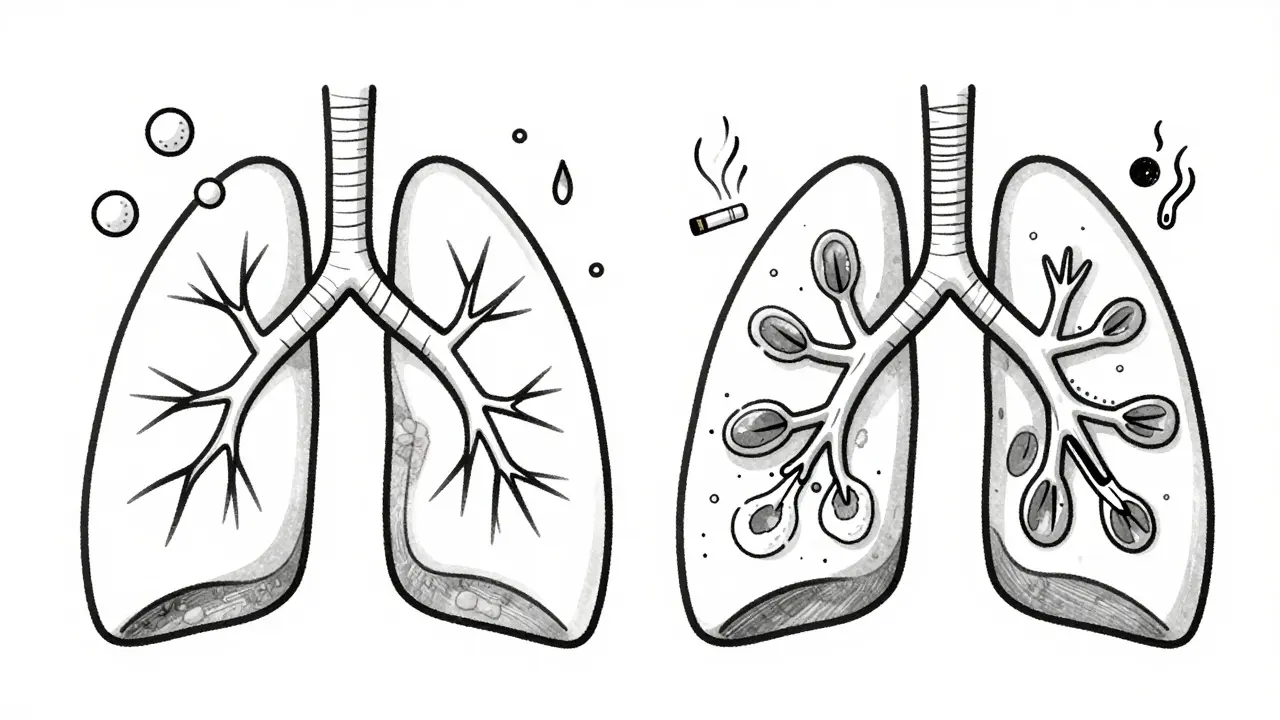
Asthma is an inflammatory condition where your airways react strongly to triggers like pollen, cold air, or exercise. The muscles around your airways tighten, swelling and mucus build up - but this is usually reversible. You might feel fine one day and struggle the next. Many people with asthma have long stretches without symptoms.
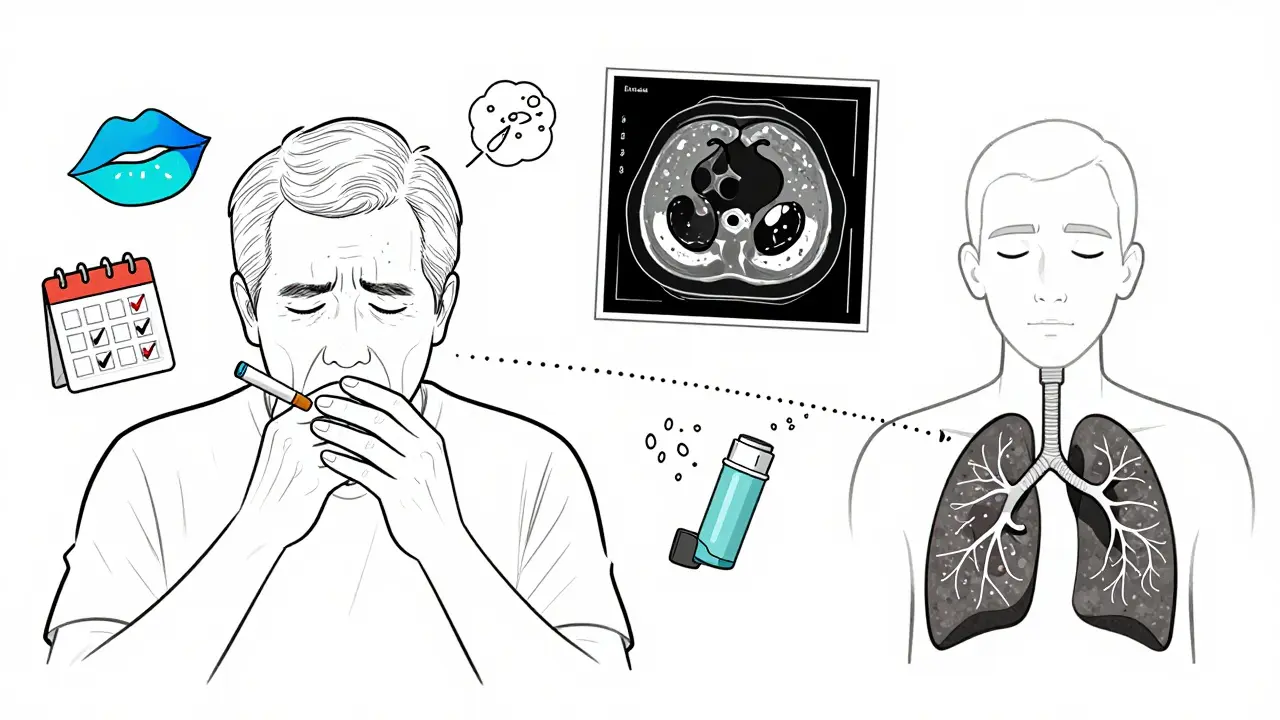
COPD, on the other hand, is damage. It’s not just inflammation - it’s permanent harm to your lungs, usually from years of smoking or long-term exposure to pollutants. The air sacs (emphysema) or airways (chronic bronchitis) are destroyed or narrowed in ways that can’t be undone. Your breathing gets worse over time, no matter what you do.
How the Symptoms Differ
Both conditions cause coughing and shortness of breath, but the pattern tells the story.
If you have asthma, your cough is often dry, especially at night or early morning. You might feel tightness in your chest before a workout or when you’re around pets. Symptoms come and go. You could go weeks without trouble - then get hit by an allergy flare-up or a cold.
COPD symptoms are constant. You’re likely to have a daily cough that brings up phlegm - often thick and colored. People with COPD don’t have symptom-free days. Even on “good” days, breathing feels harder than it used to. By the time they notice it, their lungs have already lost a lot of function.
Another clue: cyanosis. If your lips or fingernails turn blue, that’s a sign your body isn’t getting enough oxygen. This happens in about 41% of advanced COPD cases - but almost never in asthma. It’s a red flag that your lungs are failing.
Age and Risk Factors
Asthma usually starts young. Half of all cases are diagnosed before age 10. Most people are diagnosed by age 30. It’s common in kids with allergies or eczema. Genetics play a big role - if your parents have asthma, you’re more likely to get it.
COPD almost never shows up before 40. Nine out of ten cases are in people over 45. The biggest risk? Smoking. About 90% of COPD cases are tied to cigarette use. Even if you quit decades ago, the damage stays. Long-term exposure to smoke, dust, or chemical fumes also raises your risk.
Here’s something surprising: about 20% of asthma patients smoke - but smoking doesn’t cause their asthma. It just makes it worse. And if you have both asthma and a smoking history, you might actually have something called ACOS - asthma-COPD overlap syndrome. That’s a tougher condition to treat.
How Doctors Diagnose Each
A spirometry test is the gold standard. You blow hard into a tube, and the machine measures how much air you can push out and how fast.
In asthma, after you use a rescue inhaler, your numbers improve by 12% or more. That’s reversibility - and it’s a hallmark of asthma. About 95% of asthma patients show this.
In COPD, that improvement is tiny - usually less than 12%. The damage is fixed. Even after medication, your lungs don’t bounce back.
Another test: fractional exhaled nitric oxide (FeNO). If your breath has high levels of nitric oxide (above 50 ppb), it means your airways are inflamed by eosinophils - the type of inflammation seen in asthma. COPD patients usually have FeNO below 25 ppb.
Blood tests help too. Eosinophil counts above 300 cells/μL point to asthma or ACOS. Below 100? More likely pure COPD.
CT scans show the difference visually. In COPD, you’ll see holes in the lung tissue (emphysema) in 75% of cases. In asthma? Only 5% show those changes.
How They’re Treated - and Why It Matters
Asthma treatment is about controlling inflammation and preventing attacks.
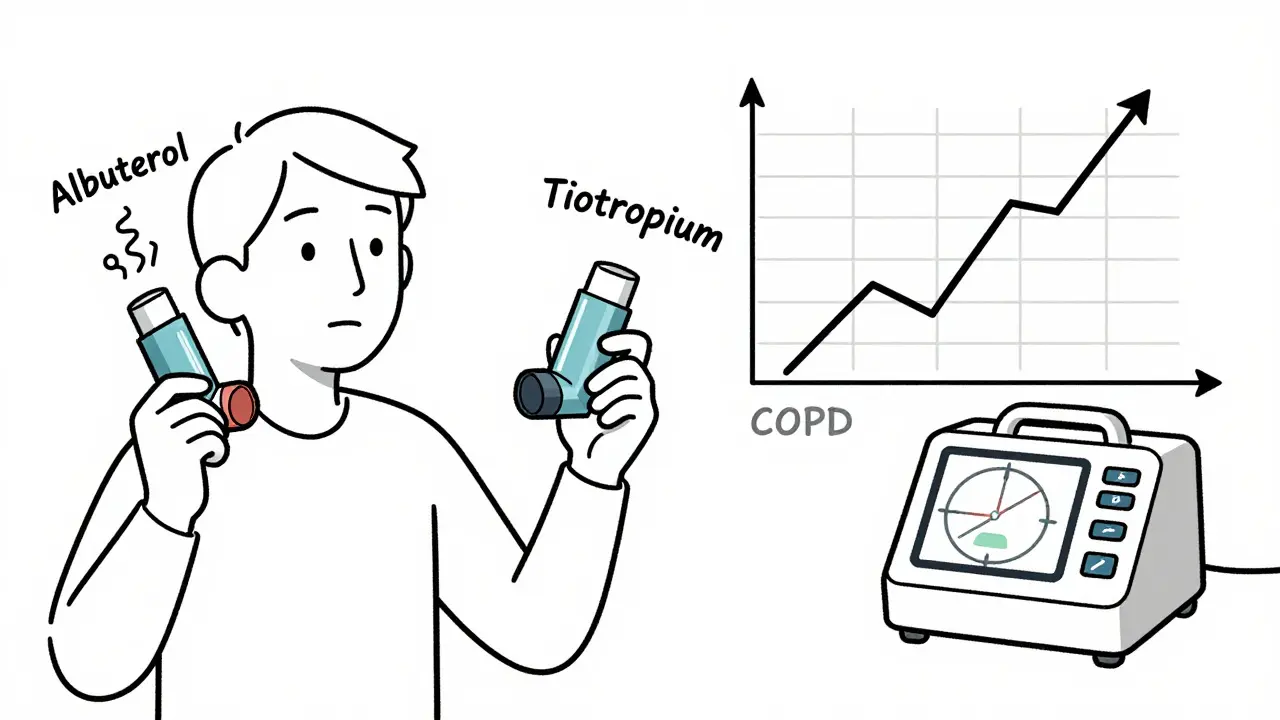
First-line: a quick-relief inhaler like albuterol for sudden symptoms. If you need it more than twice a week, you’ll likely start an inhaled corticosteroid (ICS) daily - to calm the inflammation before it flares up.
For severe asthma, biologics like omalizumab or mepolizumab target specific immune cells. These shots or infusions help about 5-10% of patients who don’t respond to standard meds. Eighty-nine percent of asthma patients get good control with the right plan.
COPD treatment is different. You don’t fix the damage - you slow it down and manage symptoms.
First-line: long-acting bronchodilators. These are either LABAs (like salmeterol) or LAMAs (like tiotropium). They relax your airways for 12-24 hours. You take them every day - even when you feel fine.
ICS? Only if you’re having frequent flare-ups. Too much steroid in COPD can increase pneumonia risk. That’s why doctors avoid it unless necessary.
Pulmonary rehab helps COPD patients more than asthma patients. After a 6-8 week program, COPD patients can walk 54 meters farther in six minutes. Asthma patients? Only 12 meters - because their baseline is already better between attacks.
What About ACOS?
Up to 25% of people with obstructive lung disease have asthma-COPD overlap syndrome (ACOS). They have features of both: chronic symptoms like COPD, but also eosinophilic inflammation like asthma.
These patients get sick more often - 1.8 emergency visits per year, compared to 0.7 for asthma alone. Their lung function declines faster.
Treatment? Usually triple therapy: a LABA, a LAMA, and an ICS. But there’s no perfect evidence for this approach. Doctors are still figuring out the best mix. If you’ve been diagnosed with one condition but aren’t improving, ask about ACOS.
Prognosis: What to Expect Long-Term
Asthma has a much better outlook. If you’re diagnosed in your 20s and manage it well, your 10-year survival rate is 92%. Many people live full lives with minimal restrictions.
COPD is more serious. Even moderate cases have a 78% 10-year survival rate. The disease keeps progressing. Hospitalizations happen more often - 0.84 per year for COPD versus 0.12 for asthma.
But quitting smoking changes everything for COPD. The Lung Health Study showed that stopping cuts disease progression by 50%. That’s huge. For asthma, smoking doesn’t cause the disease - but it makes it harder to control.
Can Asthma Turn Into COPD?
Not exactly - but long-term uncontrolled asthma can lead to permanent airway changes. About 15-20% of people with asthma for over 20 years develop fixed airflow obstruction. It looks like COPD on a test, but the root cause is still asthma-related inflammation.
This is why early, consistent treatment matters. If you’re using your rescue inhaler often, talk to your doctor. Don’t wait until your lungs are permanently damaged.
When to See a Doctor
If you’re over 40 and have a chronic cough with phlegm - especially if you’ve smoked - get checked for COPD.
If you’re under 30 and have wheezing that comes and goes with triggers like pollen or exercise - asthma is more likely.
And if you’ve been diagnosed with one, but your symptoms aren’t improving with standard treatment, ask about the other. Misdiagnosis is still common - 25% of cases over age 40 are wrong.
Don’t guess. Get tested. Your treatment - and your future - depends on it.
Can you have asthma and COPD at the same time?
Yes. This is called Asthma-COPD Overlap Syndrome (ACOS). It affects 15-25% of people with obstructive lung disease. These patients have chronic symptoms like COPD but also show signs of allergic inflammation like asthma - such as high eosinophil counts or a history of allergies. Treatment often combines long-acting bronchodilators with inhaled steroids, but it’s more complex than treating either condition alone.
Is COPD curable?
No, COPD is not curable. The lung damage - whether from emphysema or chronic bronchitis - is permanent. But it’s manageable. Quitting smoking, using prescribed bronchodilators, getting pulmonary rehab, and avoiding triggers can slow progression and help you stay active. Many people live for years with good quality of life if they follow their treatment plan.
Do inhalers work the same for asthma and COPD?
Not exactly. For asthma, short-acting inhalers (like albuterol) are the first line for quick relief, and inhaled steroids are used daily to prevent attacks. For COPD, long-acting bronchodilators (LABAs or LAMAs) are the foundation - taken every day, even when you feel fine. Steroids are added only if you have frequent flare-ups. Using asthma meds for COPD without proper guidance can be ineffective or even risky.
Can asthma go away?
Some children outgrow asthma, especially if it’s mild and triggered by viruses. But for adults, asthma is usually lifelong. Even if symptoms disappear for years, the airway sensitivity remains. A cold, stress, or smoke can trigger a flare-up. That’s why ongoing monitoring and having a rescue inhaler on hand is important - even if you feel fine.
Why do some people with asthma need shots?
These are biologic therapies - drugs like omalizumab or mepolizumab. They’re for severe asthma that doesn’t respond to inhalers. They target specific immune cells (like IgE or eosinophils) that drive inflammation. Only about 5-10% of asthma patients qualify. These shots are given every few weeks and can cut flare-ups by half. They’re not used for COPD.
Does smoking cause asthma?
Not directly. Asthma is mostly genetic or triggered by allergies. But smoking can make asthma much worse - increasing how often you have attacks and how severe they are. It also raises your risk of developing COPD. If you have asthma and smoke, quitting is the single most important thing you can do for your lungs.
How do I know if my breathing problem is serious?
If you’re using your rescue inhaler more than twice a week, waking up at night with breathing trouble, or needing emergency care for breathing issues - it’s time to see a doctor. Cyanosis (blue lips or nails), constant cough with phlegm, or feeling out of breath during simple tasks like walking to the mailbox are red flags. Don’t wait until you’re gasping - early action prevents long-term damage.





15 Comments