More than 8 million older adults in the U.S. are still taking benzodiazepines - drugs like Valium, Xanax, and Ativan - even though doctors have known for years these medications are dangerous for seniors. The numbers haven’t dropped as fast as they should. In 2023, nearly 9 out of every 100 people over 65 were prescribed one of these drugs. And about a third of them have been taking it for years. That’s not just outdated practice. It’s a public health risk.
Why Benzodiazepines Are Riskier for Seniors
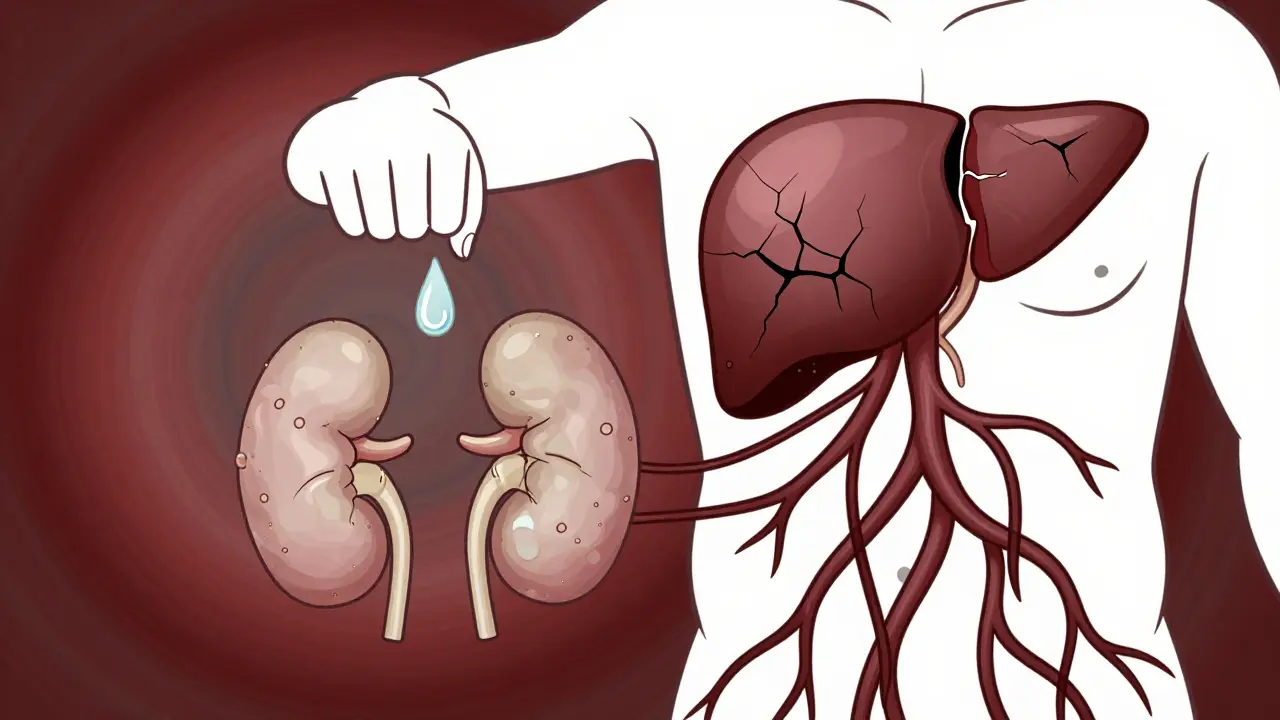
Benzodiazepines work by boosting GABA, a calming chemical in the brain. That’s why they help with anxiety and sleep - at first. But in older adults, the body doesn’t process them the same way. Liver function slows down. Kidneys filter less. Fat tissue holds onto the drugs longer. That means even small doses build up over time. The result? Drowsiness that lasts too long, dizziness that turns into falls, and memory gaps that don’t go away.
One of the most shocking facts? Taking benzodiazepines for more than six months increases the risk of Alzheimer’s disease by 84%. That’s not a small uptick. That’s nearly double the chance. And it’s not just long-term use. Even a few months of use raises the risk by 32%. The longer you take them, and the higher the dose, the worse it gets. This isn’t speculation. It’s backed by large studies from France, Canada, and the U.S., published in peer-reviewed journals.
Then there’s the fall risk. Older adults on benzodiazepines are at least 50% more likely to break a hip. Why? The drugs slow reaction time, blur balance, and weaken muscles. A 2013 study found that the motor impairment from these drugs is like driving with a blood alcohol level of 0.05% to 0.079%. That’s above the legal limit in many places. And it’s not just falls - it’s car crashes, hospital trips, and long recoveries that often never fully happen.
And here’s something most people don’t realize: these drugs don’t even work well long-term. The sleep or anxiety relief fades after a few weeks. Then the body needs more to feel the same effect. When you try to stop, the anxiety and insomnia come back worse - a rebound effect. Many seniors end up stuck, not because the drug helps, but because quitting feels impossible.
What the Experts Say - And Why It Matters
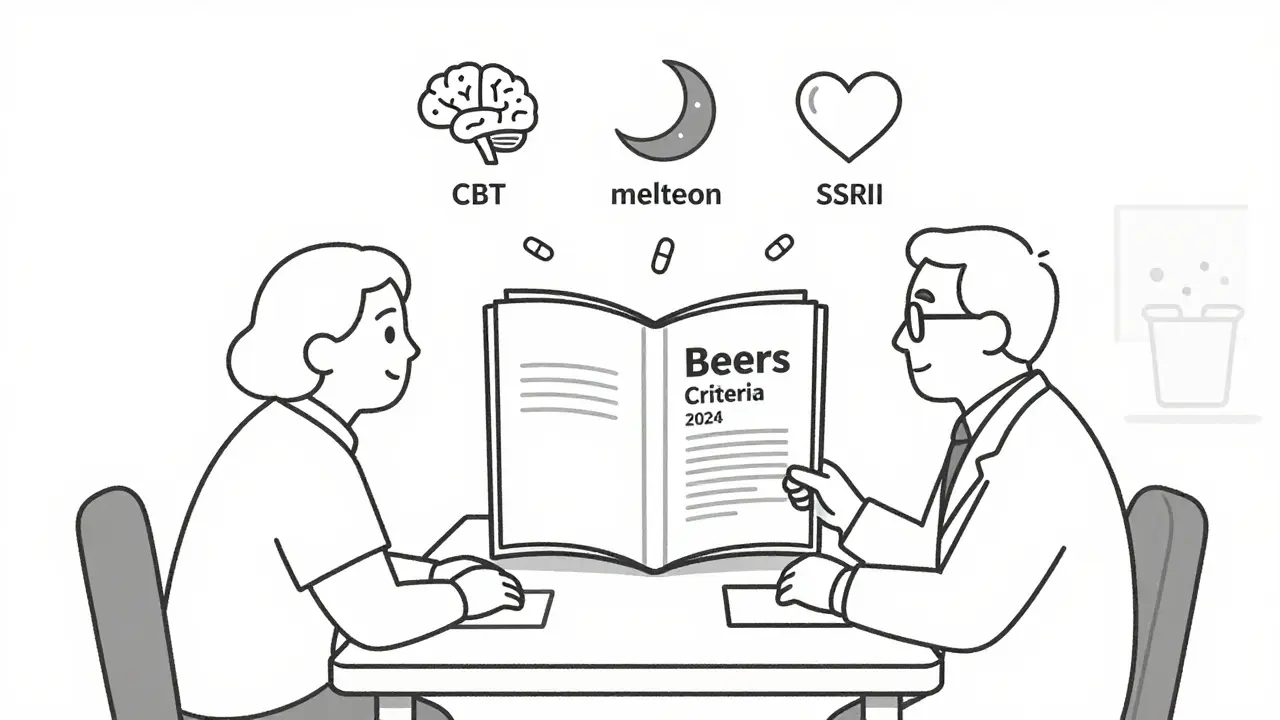
The American Geriatrics Society has listed benzodiazepines as potentially inappropriate for seniors since 2012, and updated that warning again in 2019 and 2024. Their Beers Criteria is the gold standard. It’s not a suggestion. It’s a warning signed off by hundreds of geriatric specialists.
Dr. Sharon Inouye from Harvard calls them “among the most dangerous medications for older adults.” Dr. Michael Steinman from UCSF says even short-term use carries underestimated risks. Dr. Malaz Boustani’s research found a 51% higher dementia risk in long-term users. These aren’t isolated opinions. They’re the consensus.
And it’s not just doctors. The FDA added new warnings to all benzodiazepine labels in April 2024, requiring them to state clearly: “Use in elderly patients may increase the risk of dementia.” Medicare now flags prescriptions for review under its Drug Utilization Review program. Pharmacies are supposed to alert prescribers when someone over 65 gets a long-term benzodiazepine script.
Despite all this, many seniors still believe these drugs are safe because their doctor prescribed them. A Reddit user who works in geriatric nursing said she sees it every week: “Nine out of ten seniors think their Xanax is harmless.” That’s the gap. The science says one thing. The perception says another.
The Safer Alternatives - What Actually Works
There are better options. And they don’t come with a risk of dementia or broken hips.
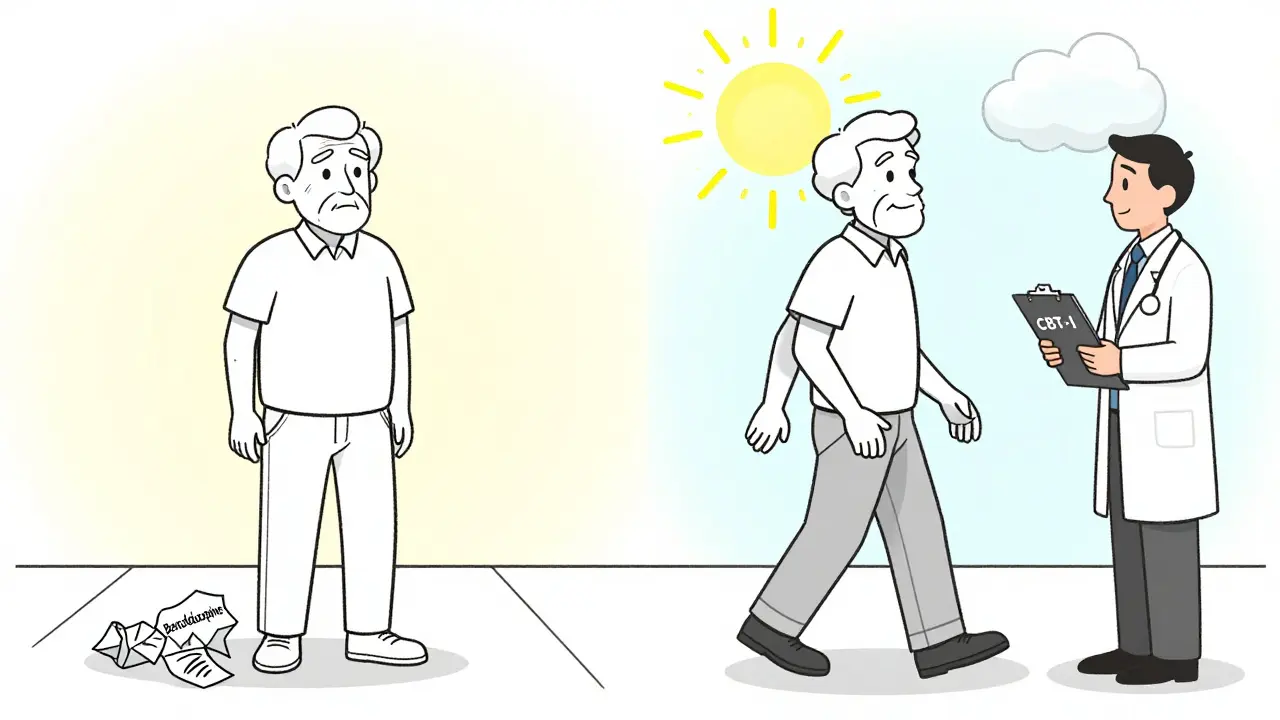
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective treatment for chronic sleep problems in older adults. Studies show 70-80% of seniors who do CBT-I improve their sleep - and keep those gains for years. Unlike pills, it doesn’t wear off. It rewires how the brain thinks about sleep. Medicare started covering CBT-I in 2022. But only 12% of eligible seniors are using it. Why? Too few providers offer it. Too many patients don’t know it exists.
SSRIs and SNRIs - like sertraline, escitalopram, or venlafaxine - are now first-line for anxiety in seniors. They take 4 to 6 weeks to work. That’s slower than Xanax. But they don’t cause dizziness, memory loss, or addiction. They’re safe for long-term use. And they help with both anxiety and depression, which often go together in older adults.
Ramelteon is a melatonin receptor agonist. It helps with falling asleep, without the hangover effect or dependence risk. It’s not perfect - it doesn’t help much with staying asleep - but it’s miles safer than benzodiazepines.
And avoid antihistamines like diphenhydramine (Benadryl) or doxylamine. They’re in many over-the-counter sleep aids. But they block acetylcholine - a brain chemical critical for memory. Long-term use of these drugs increases dementia risk by up to 50%. They’re not safer. They’re just less talked about.
How to Stop - Safely
If you or a loved one is on a benzodiazepine, quitting isn’t about willpower. It’s about planning.
The American Society of Addiction Medicine recommends tapering slowly - 5% to 10% of the dose every one to two weeks. For some, that means 8 weeks. For others, 6 to 12 months. Going too fast can trigger seizures, panic attacks, or severe insomnia.
Success rates jump when tapering is paired with CBT. One study found 65% of seniors successfully stopped their benzodiazepine when they got CBT support. Without it? Only 35% made it.
Here’s what to ask your doctor:
- What’s the reason I’m still on this drug?
- What are the risks if I keep taking it?
- What are the risks if I stop?
- What non-drug options are available to me?
- Can we make a step-by-step plan to reduce this, with check-ins every two weeks?
Don’t wait for your next annual visit. Schedule a dedicated appointment. Bring a list of all your meds. Ask for a copy of the Beers Criteria. Most doctors will agree - if you come prepared.
What’s Changing in 2025 and Beyond
The tide is turning. CMS launched the Beers Criteria Action Plan in January 2025, aiming to cut inappropriate benzodiazepine use by 50% by 2027. They’re training pharmacists, updating electronic health records, and requiring patient counseling before long-term scripts are filled.
The NIH is funding a five-year trial called BRIGHT - Benzodiazepine Reduction in Geriatric Health Through Telehealth. It’s testing if remote coaching, apps, and virtual therapy can help seniors quit safely. Results won’t be in until 2029, but early pilot data is promising.
And the American Geriatrics Society has made benzodiazepine deprescribing one of its top five priorities for 2025-2027. They’re creating patient decision aids - simple tools that explain risks and alternatives in plain language.
The message is clear: benzodiazepines are not a long-term solution for seniors. They’re a short-term bandage with long-term consequences.
What Patients Are Saying
On Drugs.com, WebMD, and GoodRx, seniors gave benzodiazepines an average rating of 5.2 out of 10 for use in older adults. Compare that to non-benzodiazepine alternatives - they average 7.8.
Positive reviews often say: “It helped me get through a rough patch.”
Negative ones say: “I felt like I was walking through fog every day.” “I fell three times in six months.” “I couldn’t stop, even though I knew it was hurting me.”
One woman wrote: “I stopped my lorazepam after 12 years. The first week was hell. But after three months, I could remember my grandson’s name without asking my daughter to remind me.”
That’s the difference.
Are benzodiazepines ever safe for seniors?
They can be used for very short-term situations - like severe anxiety before surgery, or acute panic attacks. But even then, they should be given in the lowest possible dose for no more than a few days. Long-term use - even for weeks - is not recommended. The Beers Criteria and FDA agree: for chronic anxiety or insomnia, the risks outweigh the benefits.
Can I stop benzodiazepines cold turkey?
No. Stopping suddenly can cause seizures, hallucinations, extreme anxiety, or rebound insomnia. Withdrawal symptoms affect 60-80% of long-term users. Always work with a doctor to create a slow taper plan. Most seniors need 8 to 16 weeks, sometimes longer. Never reduce your dose without medical supervision.
What’s the best non-drug treatment for anxiety in seniors?
Cognitive Behavioral Therapy (CBT) is the most effective. It teaches practical skills to manage anxious thoughts and physical symptoms. CBT for insomnia (CBT-I) is equally powerful for sleep problems. Both are covered by Medicare, though access is still limited. Look for therapists trained in geriatric CBT - they understand how aging affects mood and thinking.
Do all benzodiazepines carry the same risk?
Yes. The 2024 Beers Criteria update made it clear: all benzodiazepines - whether short-acting like lorazepam or long-acting like diazepam - pose serious risks in older adults. Long-acting ones build up more in the body, but even short-acting ones can cause falls, memory loss, and increased dementia risk. There’s no “safer” benzodiazepine for seniors.
How do I know if my parent is dependent on benzodiazepines?
Signs include needing higher doses over time, feeling worse when they miss a dose, avoiding social events because they feel “off,” or becoming confused or unsteady after taking the pill. If they’ve been on it for more than three months, dependence is likely. Talk to their doctor about a taper plan - don’t assume it’s normal aging.
Are there support groups for seniors quitting benzodiazepines?
Yes. The Benzodiazepine Information Coalition has over 12,500 members and offers online forums, webinars, and peer support. Many local Area Agencies on Aging also run support groups. While access is harder in rural areas, telehealth options are expanding. You don’t have to quit alone.
What to Do Next
If you’re on a benzodiazepine: make an appointment with your doctor. Bring this article. Ask about CBT-I or an SSRI. Ask about tapering.
If you’re caring for someone who is: track their doses. Note any falls, confusion, or memory lapses. Don’t wait for a crisis. Start the conversation now.
If you’re a clinician: review your elderly patients’ med lists. Flag long-term benzodiazepine use. Offer alternatives. Use the Beers Criteria as your guide.
The goal isn’t to scare people. It’s to give them better choices. Seniors deserve sleep without fog. Calm without risk. Safety without stigma. And there are real, proven ways to get there - without pills that could steal their memory.







9 Comments