Every year, more than 1.5 million people in the U.S. end up in the emergency room because of medication mistakes. Many of these aren’t accidents-they’re preventable. The biggest reason? Patients don’t know the language their doctors and pharmacists use to keep them safe. You don’t need a medical degree to protect yourself. You just need to understand a few key terms-and know how to use them.
What Are the Eight Rights of Medication Safety?
The foundation of medication safety isn’t a complicated algorithm or a high-tech app. It’s a simple checklist called the Eight Rights. These aren’t suggestions. They’re your rights as a patient. If you don’t hear them used in your care, ask for them.
- Right patient - They must confirm your identity using two things: your full name and your date of birth. Don’t let them skip this. I’ve seen nurses call out names in a hallway and hand a pill to the wrong person. It happens.
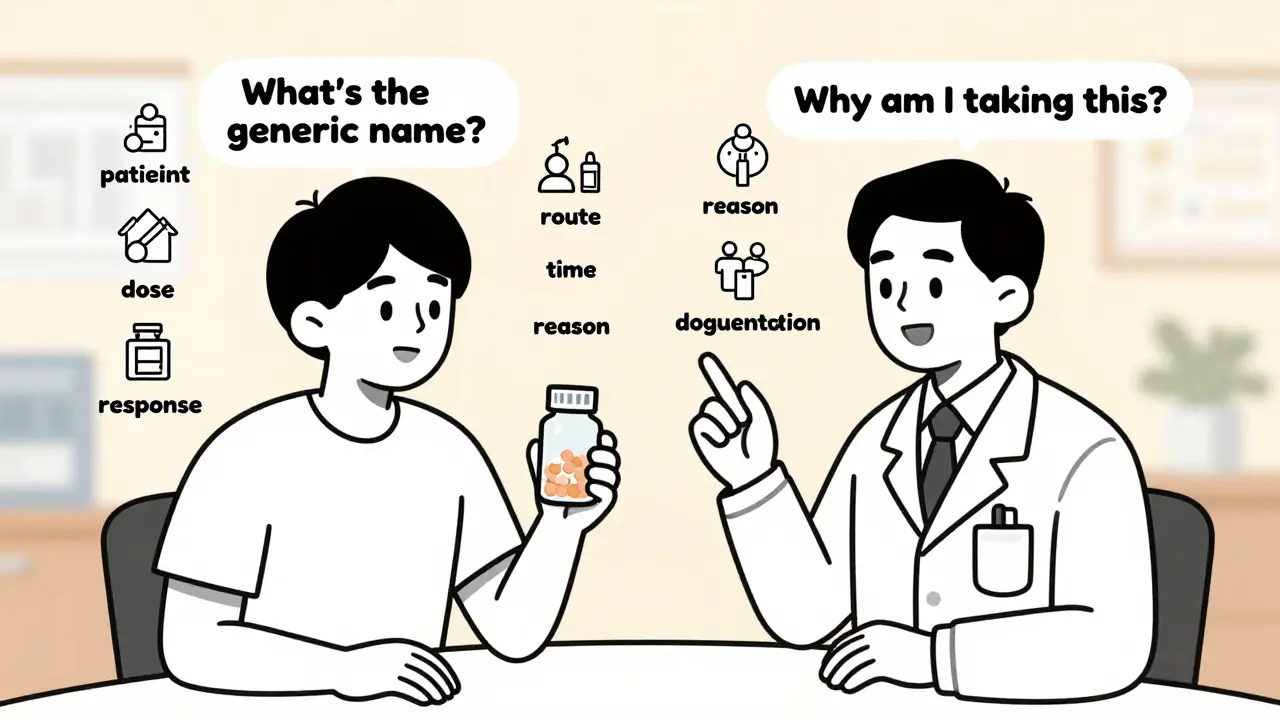
- Right medication - Ask for both the brand name and the generic name. If your prescription says "Lisinopril," but the bottle says "Zestril," that’s the same thing. But if it says "Lisinopril" and you were supposed to get "Lisinopril-HCTZ," that’s a problem. Similar-sounding names cause 23% of medication errors.
- Right dose - Know how much you’re supposed to take. If it’s a liquid, ask how many milliliters or teaspoons. Kids are especially at risk-15% of pediatric errors come from wrong dosing. Don’t guess. Use the measuring cup that came with the medicine.
- Right route - Is it meant to be swallowed, injected, applied to the skin, or inhaled? I’ve seen people accidentally swallow an IV medication because they didn’t know the difference. That’s deadly. Always ask: "How is this supposed to go in?"
- Right time - Is it morning, night, with food, or on an empty stomach? Taking a blood pressure pill at night when it’s meant for morning can crash your pressure. Use a phone alarm or a pill organizer. Studies show this cuts dosing errors by 31%.
- Right reason - This one’s critical. Why are you taking this? Not just "for high blood pressure," but "to lower your systolic pressure so your heart doesn’t get overworked." If your doctor can’t explain it simply, you’re not getting enough info. Patients who ask this question reduce inappropriate prescriptions by 28%.
- Right documentation - Make sure every time you get a medication, it’s written down. At the hospital, ask: "Did you record that I got this?" At the pharmacy, check your profile online. If it’s not documented, it didn’t happen.
- Right response - What should you feel? What side effects are normal? What’s a red flag? If you’re on a blood thinner and you start bruising easily, that’s a response to track. If you’re on a new antidepressant and you feel worse after two weeks, that’s a response to report. Tracking this cuts severe reactions by 35%.
What Is an Adverse Drug Event (ADE)?
An ADE isn’t just a side effect. It’s when a medicine harms you. That includes allergic reactions, overdoses, interactions, and mistakes. If you take a drug you’re allergic to, that’s an ADE. If you take two pills instead of one and get dizzy, that’s an ADE. If your blood pressure drops too low because you took your pill with grapefruit juice, that’s an ADE.
The CDC says ADEs are one of the top preventable problems in healthcare. And most happen because someone didn’t know what to watch for. You don’t need to memorize every possible side effect. Just know this: if something feels wrong, new, or worse than expected-speak up. Don’t wait. Don’t assume it’s "normal."
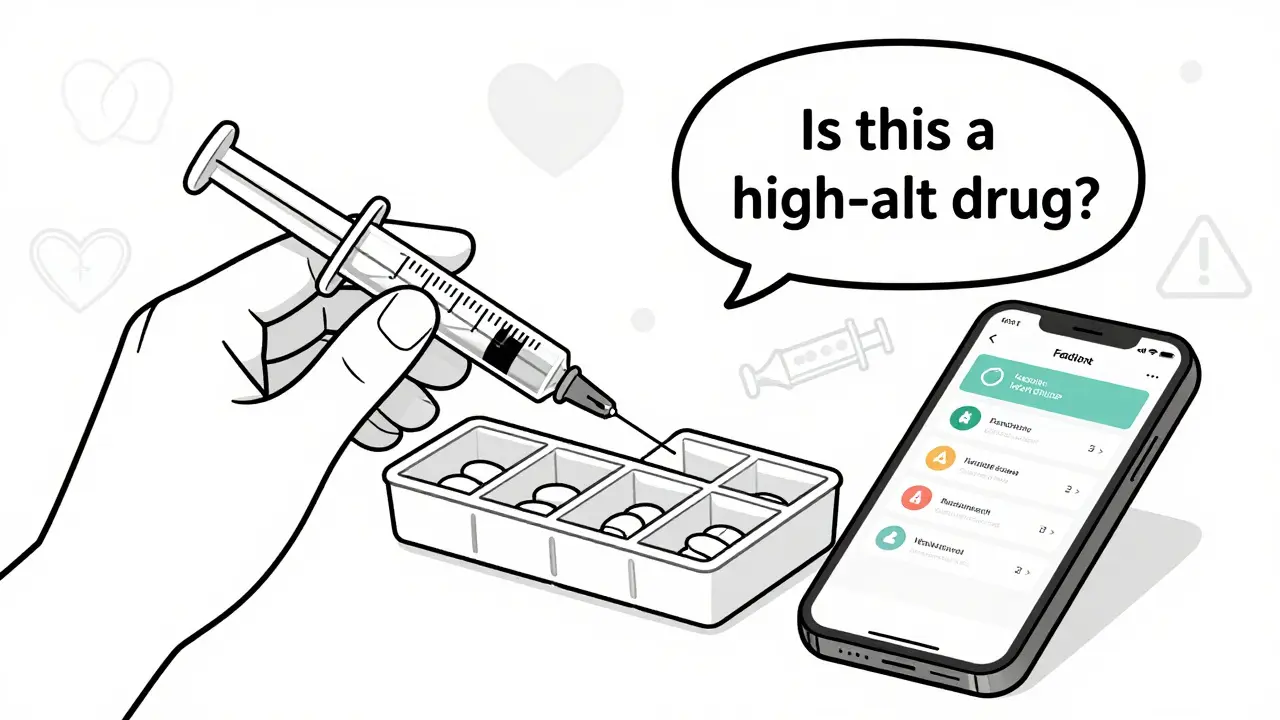
What Are High-Alert Medications?
Some drugs are like loaded guns. If used wrong, they can kill. These are called high-alert medications. The Institute for Safe Medication Practices (ISMP) lists them: insulin, blood thinners like warfarin, opioids like morphine, IV potassium, and sedatives for ICU patients.
These aren’t rare. One in three hospital patients gets at least one. And they’re behind 67% of fatal medication errors. That doesn’t mean you shouldn’t take them. It means you need to be extra careful.
Ask: "Is this a high-alert drug?" Then ask: "What should I watch for?" If you’re going home with insulin, make sure you know how to store it, how to inject it, and what low blood sugar feels like. If you’re on warfarin, know which foods to avoid and why you need regular blood tests. Don’t let the pharmacy hand you a bottle and say, "Read the label." That’s not enough.
What’s a Close Call?
A close call is when something almost went wrong-but didn’t. You were about to take the wrong pill, but you caught it. The nurse almost gave you the wrong dose, but checked the chart. That’s not luck. That’s awareness.
Most people don’t report close calls. They think, "Good thing nothing happened." But close calls are the early warning signs. If you notice one, tell your doctor or pharmacist. They need to know. These reports help fix system flaws before someone gets hurt.
What Are Sentinel Events?
A sentinel event is the worst-case scenario: death or serious injury caused by a medication error. The Joint Commission defines it as something that shouldn’t happen in a safe system. A patient dies because they got the wrong drug. A baby is harmed because the dose was 10 times too high. These aren’t accidents. They’re failures.
Knowing this term isn’t about fear. It’s about accountability. If you hear a doctor say, "This was a sentinel event," you know they’re taking it seriously. And if you’re ever in a situation where something went badly, you have the right to ask: "Was this a sentinel event? What’s being done to make sure it doesn’t happen again?"
How Do You Use These Terms in Real Life?
You don’t need to sound like a nurse. You just need to be clear and persistent.
When you get a new prescription:
- Ask: "What’s the generic name? What’s it for?" (Right medication, right reason)
- Ask: "Is this a high-alert drug?"
- Ask: "What should I do if I feel dizzy, nauseous, or weak?" (Right response)
- Ask: "Should I take this with food? At what time?" (Right time, right route)
- Write it down. Or use an app like Medisafe-used by over 8 million people-to track doses and alerts.
At the hospital:
- Before they give you any pill, ask: "Can you confirm my name and date of birth?" (Right patient)
- Ask: "Why am I getting this now?" (Right reason)
- Ask: "Is this documented in my chart?" (Right documentation)
At the pharmacy:
- Compare the bottle label to your prescription. If the name or dose looks off, say so.
- Ask: "Is this the same as what my doctor ordered?"
Why This Matters More Than Ever
In 2024, the Joint Commission made it mandatory for hospitals to teach patients the Eight Rights before discharge. The CDC and FDA set a goal: by 2030, 90% of patients should know at least five of these terms. Right now, only 43% do.
Why the push? Because it works. Studies show patients who use these terms cut their risk of harm by up to 50%. That’s not a small number. That’s life or death.
And it’s not just about being "informed." It’s about being empowered. You’re not a passive recipient of care. You’re the most important person in your own safety team. No one else will check every pill, every time. But you can.
What If You Don’t Understand?
Health literacy is a real barrier. The National Assessment of Adult Literacy found only 12% of U.S. adults can easily understand complex medical instructions. If you don’t get it, say so. Ask for simpler words. Ask for pictures. Ask for a family member to come with you.
Many clinics now offer multilingual safety guides. Ask if they have them. If not, request them. Your voice matters.
You don’t need to be perfect. You just need to be curious. Ask one question. Write one thing down. Double-check one pill. That’s how safety starts.
What’s the most important medication safety term I should remember?
The most important term is "right reason." If you don’t know why you’re taking a medication, you can’t tell if it’s working-or if it’s dangerous. Asking "Why am I taking this?" is the single most effective way to prevent inappropriate prescriptions and avoid drug interactions.
Can I ask my pharmacist to explain the Eight Rights?
Yes, absolutely. Pharmacists are trained to help you understand your meds. They see hundreds of prescriptions a day. If you’re confused about the dose, route, or reason, ask them. They’re not there just to hand out pills-they’re your safety backup.
What should I do if I think I got the wrong medicine?
Don’t take it. Call your pharmacy right away. Have your prescription number and the name of the medicine ready. Compare the label to your doctor’s instructions. If there’s a mismatch, ask them to confirm with your doctor. Never guess. Never assume. It’s better to be safe than sorry.
Are over-the-counter meds included in these safety rules?
Yes. Many ADEs come from OTC drugs like ibuprofen, cold medicines, or sleep aids. They’re not harmless just because you don’t need a prescription. Taking too much acetaminophen can cause liver failure. Mixing cold meds with antidepressants can be deadly. Always check with your pharmacist before adding any OTC drug to your routine.
How can I keep track of all my meds?
Use a simple list: medicine name, dose, reason, time to take, and doctor’s name. Keep it in your wallet or phone. Apps like Medisafe, MyTherapy, or even a notes app work. Update it every time something changes. Bring it to every appointment. It’s your personal safety checklist.



13 Comments