Warfarin-Antibiotic Interaction Checker
Select an antibiotic to see its interaction risk with warfarin and recommended monitoring steps.
When you're on warfarin, even a simple course of antibiotics can throw your blood thinning off balance-sometimes dangerously. This isn't just a theoretical risk. Every year, tens of thousands of people on warfarin get prescribed antibiotics for infections, and a significant number end up with bleeding complications because their INR spikes without warning. The truth? You don’t need to avoid antibiotics. But you do need to know which ones are risky, how to monitor for problems, and what to do when things go sideways.
Why Warfarin and Antibiotics Don’t Mix Quietly
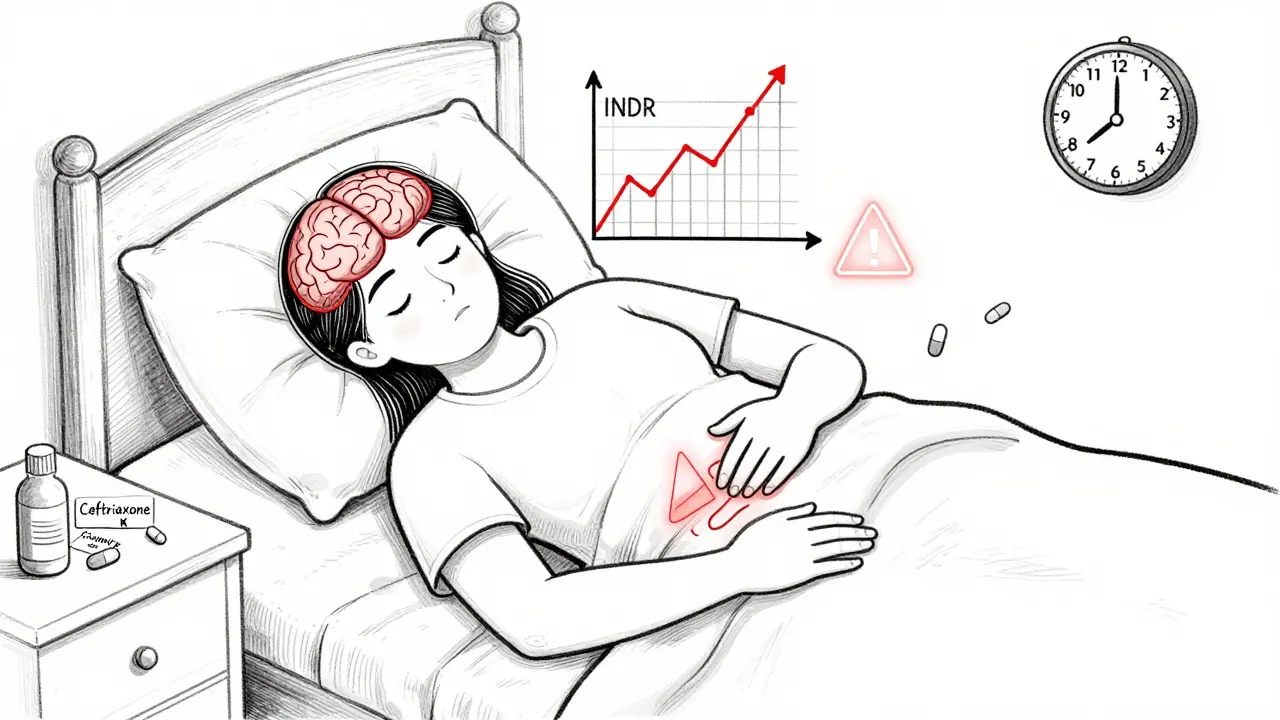
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s precise. Too little, and you risk clots. Too much, and you bleed. Its narrow window-target INR between 2.0 and 3.0-means even small changes can tip the scale. Antibiotics interfere in three main ways, and you need to understand all of them.First, some antibiotics shut down the liver enzyme CYP2C9, which breaks down the active part of warfarin. When this enzyme slows down, warfarin builds up in your blood. Drugs like trimethoprim-sulfamethoxazole (Bactrim), ciprofloxacin, and erythromycin are strong offenders here. Second, antibiotics wipe out gut bacteria that make vitamin K. Even if your diet is fine, your body loses a steady 10-15% of its vitamin K supply. That’s enough to make your INR climb, especially with broad-spectrum antibiotics like ceftriaxone. Third, some antibiotics like Bactrim bind tightly to proteins in your blood, pushing warfarin off those proteins and making more of it free and active right away.
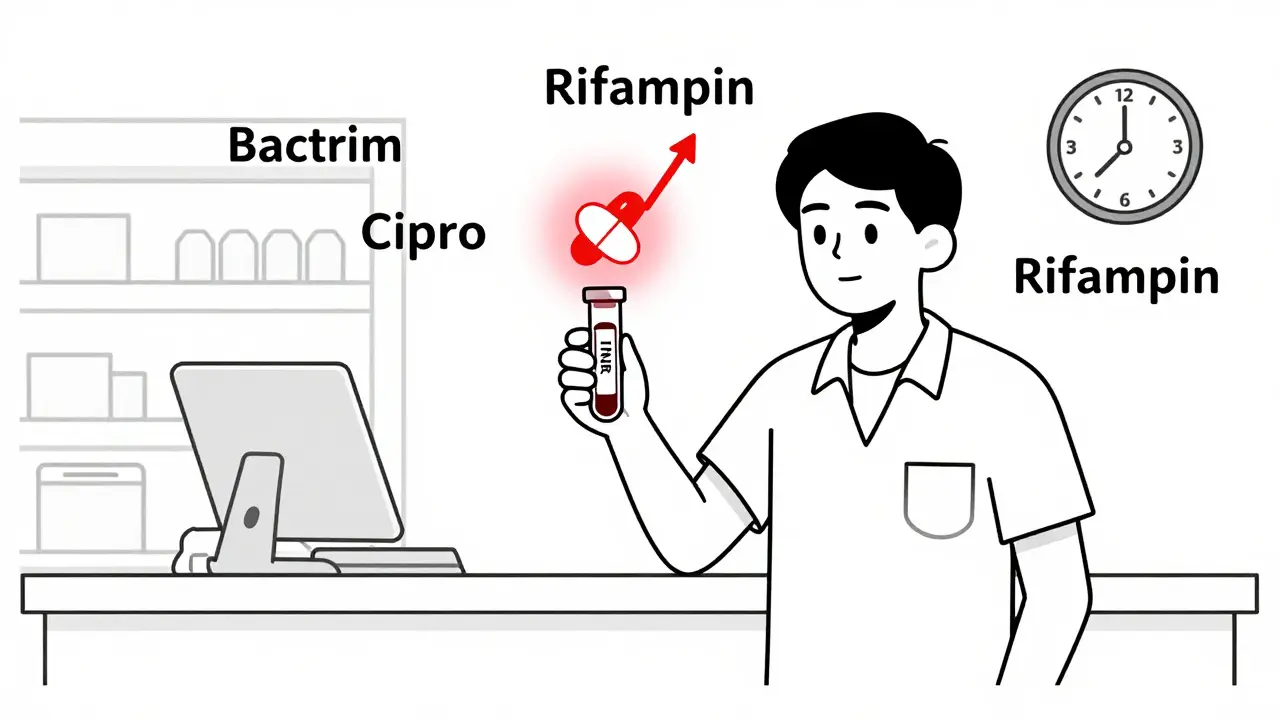
And then there’s the exception: rifampin. Instead of blocking warfarin’s breakdown, it speeds it up. If you start rifampin, your INR will drop. That’s just as dangerous-clots can form fast. You’ll need a higher warfarin dose, and it takes weeks to stabilize.
Which Antibiotics Are High Risk?
Not all antibiotics are created equal when you’re on warfarin. Some barely touch your INR. Others? They’re red flags.- High risk (INR spike >1.5 units): Trimethoprim-sulfamethoxazole (Bactrim), fluconazole (Diflucan). Bactrim is the biggest concern. Studies show it triples the risk of hospitalization for bleeding. Many clinicians cut warfarin doses by 25-50% when starting it.
- Moderate risk (INR spike 0.5-1.5 units): Ciprofloxacin, levofloxacin, amoxicillin, azithromycin (sometimes), clarithromycin, ceftriaxone. These are common. You’ll need closer monitoring.
- Low risk (minimal effect): Clindamycin, metronidazole (in most cases), azithromycin. These are often preferred for patients on warfarin, especially for dental work or skin infections.
Here’s the catch: even low-risk antibiotics can cause issues in older adults, those with liver disease, or people already on the edge of their target INR. There’s no universal rule-just probabilities.
What Happens When You Take Them Together?
Timing matters. You won’t see a change in your INR the day you start an antibiotic. It takes time.For antibiotics that inhibit CYP2C9 (like Bactrim or ciprofloxacin), INR usually starts rising within 2-3 days and peaks around day 5. For those that kill vitamin K-producing bacteria (like ceftriaxone), it’s slower-INR climbs over 3-7 days. With rifampin, the opposite happens: INR drops after 3-5 days and keeps falling for weeks.
One study tracked over 128,000 elderly patients on warfarin. Those who took any antibiotic had more than double the risk of bleeding that sent them to the hospital. With Bactrim? The risk jumped to more than three times higher. But here’s the nuance: most people didn’t bleed. The absolute risk is still low. That’s why blanket avoidance isn’t the answer-it’s about smart monitoring.
What You Should Do Before Starting an Antibiotic
Don’t wait for symptoms. Don’t assume your doctor will catch it. Take control.- Check your INR right before you start the antibiotic. Write it down.
- Tell your pharmacist you’re on warfarin. They’ll flag interactions you might miss.
- Ask: “Is there a lower-risk antibiotic I can use instead?” Clindamycin is often a safe substitute for dental or skin infections.
- Don’t stop your warfarin. Stopping increases clot risk-sometimes fatally.
For high-risk antibiotics like Bactrim, many clinics recommend reducing your warfarin dose by 25-50% as a precaution. But that’s not one-size-fits-all. A 75-year-old with atrial fibrillation and a history of falls might need a bigger cut than a 50-year-old who’s otherwise healthy.
When to Check Your INR After Starting an Antibiotic
The standard advice: check within 3-5 days. But that’s the bare minimum.If you’re on a high-risk antibiotic like Bactrim or fluconazole, get your INR checked at day 3 and again at day 5. If you’re on a moderate-risk one like amoxicillin or ciprofloxacin, check at day 5-7. For rifampin, check every 1-2 weeks for at least 6-8 weeks. Your dose will need multiple adjustments.
Don’t wait for bruising or nosebleeds. By then, it’s too late. A silent INR of 6.0 can lead to internal bleeding before you feel a thing. That’s why routine monitoring saves lives.
What to Do If Your INR Goes Too High
If your INR is 4.0-5.0 and you have no bleeding: skip your next warfarin dose, then resume at a lower dose. Your doctor might give you a small amount of vitamin K orally.If your INR is 5.0-9.0 and you have minor bleeding (bruising, nosebleeds): skip warfarin for 1-2 doses, take vitamin K, and monitor daily.
If your INR is over 9.0 or you have serious bleeding (vomiting blood, black stools, severe headache): go to the ER immediately. You may need IV vitamin K, fresh frozen plasma, or other emergency measures.
Never panic. Don’t stop warfarin cold. Don’t try to “fix” it yourself with vitamin K supplements without medical advice. Too much vitamin K can undo your therapy for weeks.
Dental Visits and Surgery: Special Considerations
Dentists often prescribe antibiotics before procedures to prevent infection. But for people on warfarin, this is where things get tricky.Research shows that for most dental work, antibiotics aren’t even needed. If they are, clindamycin is the safest bet. Avoid amoxicillin if your INR is already high. For minor procedures like fillings or cleanings, you usually don’t need to adjust warfarin at all. For major surgery? Your doctor might temporarily switch you to heparin injections for a few days, then restart warfarin after.
One study found that patients on warfarin who had dental extractions without stopping their medication had no more bleeding than those who stopped it. The key? Good technique and tight INR control before the procedure.
The Bigger Picture: Monitoring Beats Fear
It’s tempting to think antibiotics and warfarin should never mix. But that’s not realistic. People need antibiotics. They need to stay on warfarin. The goal isn’t avoidance-it’s management.A 2014 study of nearly 40,000 warfarin patients found that those who took antibiotics had no higher risk of stroke, clotting, or death than those who were sick but didn’t get antibiotics. The real danger? Not checking INR. Not adjusting doses. Not communicating between doctors.
The bottom line: if you’re on warfarin and need an antibiotic, you’re not doomed. You’re just one conversation away from safety. Tell your doctor. Ask for the INR check. Know the signs of bleeding. And don’t assume everything will be fine because you’ve been on warfarin for years. Every new drug changes the game.
What Your Pharmacist Can Do for You
Your pharmacist is your hidden ally. They see every prescription you fill. They know which drugs interact with warfarin better than most doctors do.Ask them: “Is this antibiotic safe with my warfarin?” They can flag risks you didn’t know about. They can suggest alternatives. They can tell you when to check your INR. Many pharmacies offer free INR monitoring for patients on warfarin. Use it.
Don’t just pick up your script and go. Spend two minutes asking questions. It’s not being difficult-it’s being smart.





13 Comments