When you take one sedative, your body slows down a little. Take two, and it slows down more. Take three or more-and you might not wake up. This isn’t science fiction. It’s what happens when people combine CNS depressants like opioids, benzodiazepines, alcohol, or sleep meds. The risks aren’t just theoretical. They’re deadly, and they’re happening every day.
What Happens When Sedatives Mix?
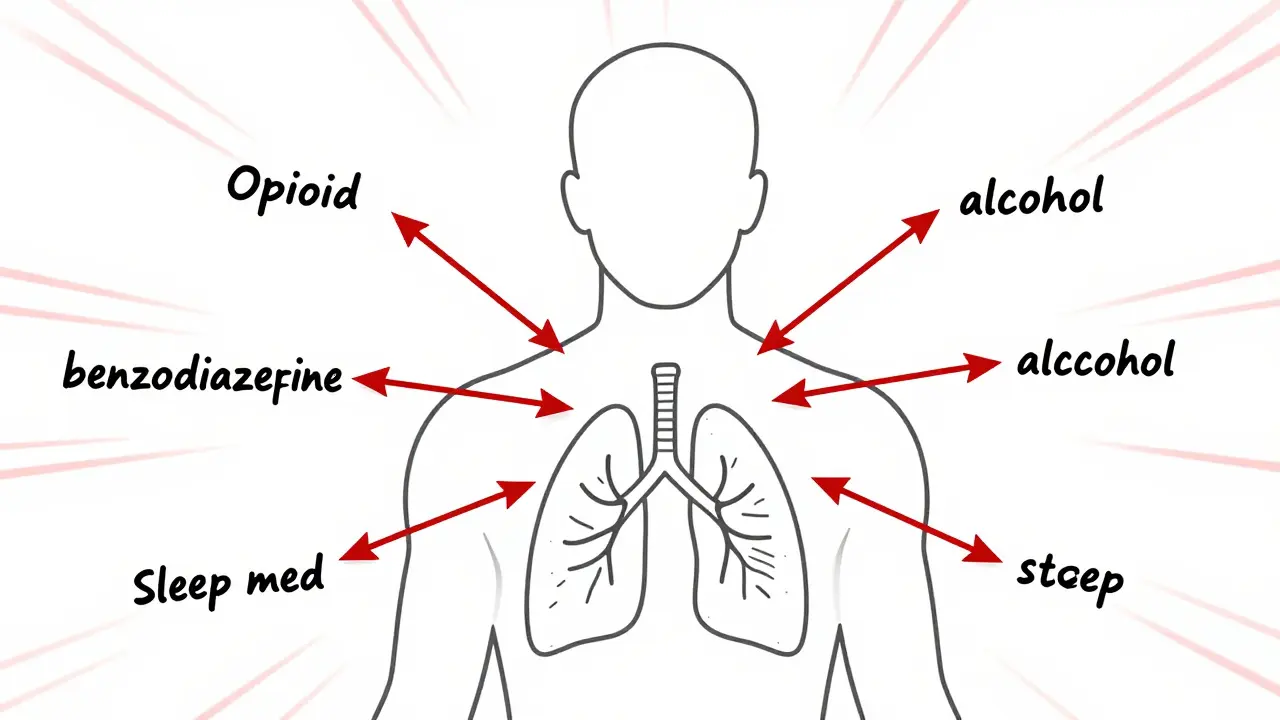
Central nervous system (CNS) depressants work by boosting GABA, a brain chemical that calms neural activity. That’s why they help with anxiety, insomnia, or seizures. But when you stack them-say, taking oxycodone for pain while also using alprazolam for panic attacks-their effects don’t just add up. They multiply. This is called synergistic depression. Your breathing slows. Your heart rate drops. Your brain stops signaling your lungs to work.
The FDA warned in 2016 that combining opioids and benzodiazepines increases the risk of fatal overdose by 2.5 to 4.5 times. That’s not a small bump. It’s a cliff. Studies show respiratory rates can plummet from a normal 12-20 breaths per minute to as low as 4-6. Oxygen saturation can drop below 85% in under 20 minutes. At that point, brain damage starts. In four to six minutes without oxygen, cells begin dying. Many people never make it to the hospital.
Who’s Most at Risk?
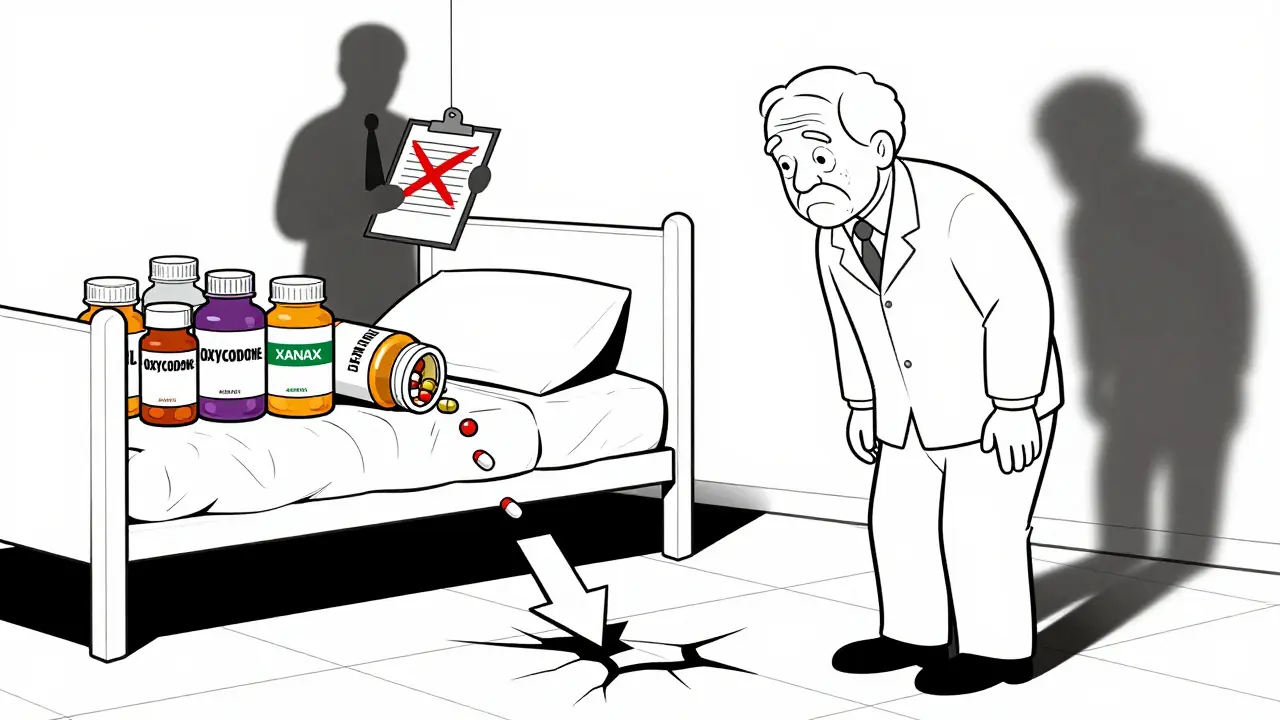
It’s not just people using drugs recreationally. The biggest danger is among patients prescribed these meds legally. A 2012 study found nearly 30% of people on long-term opioid therapy were also taking benzodiazepines-even without a history of substance use. That number jumped to 39% among those with past addiction. Women are 1.7 times more likely to be prescribed these combinations. People with depression are more than twice as likely. Elderly patients? They’re at the highest risk of all.
Older adults metabolize drugs slower. Their brains are more sensitive. Even low doses can cause extreme dizziness, confusion, and loss of balance. Research shows elderly patients on three or more CNS depressants are 2.8 times more likely to fall and 3.4 times more likely to suffer a hip fracture. The American Geriatrics Society lists 34 sedatives as potentially inappropriate for seniors because of this exact danger. Yet many doctors still prescribe them together.
Common Dangerous Combinations
You might not realize you’re mixing dangerous drugs. Here are the most common-and deadly-pairings:
- Opioids + benzodiazepines: This is the most studied and deadliest combo. Think hydrocodone + diazepam or oxycodone + lorazepam. Even short-term use raises overdose risk sharply.
- Opioids + alcohol: A glass of wine with your pain pill? That’s not harmless. Alcohol boosts opioid effects, making breathing suppression worse. One study found 12-13% of chronic opioid users drank within two hours of taking their dose.
- Benzodiazepines + sleep meds: Zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata) are all CNS depressants. Taking them with Xanax or Klonopin multiplies drowsiness and impairs coordination.
- SSRIs + CNS depressants: Many antidepressants like fluoxetine or sertraline interfere with liver enzymes that break down sedatives. This causes drugs to build up in the bloodstream, increasing overdose risk even at normal doses.
And it’s not just pills. Over-the-counter sleep aids like diphenhydramine (Benadryl, Tylenol PM) are antihistamines with strong sedative effects. Mixing them with prescription meds? That’s another hidden risk.
Long-Term Consequences
Even if you don’t overdose, long-term use of multiple sedatives wears your body down. Chronic users report:
- Weight gain of 12-18 pounds in a year
- Chronic fatigue affecting 45% of users
- Sexual dysfunction in 32%
- Sleep apnea in 27%
- Depression in 38%
- Suicidal thoughts in 19% after six months
Long-term cognitive decline is another silent threat. A 2009 study tracked elderly patients and found that using multiple CNS depressants-even for months-led to a 5-point drop on memory tests. That’s the difference between living independently and needing help with daily tasks.
Why Do Doctors Still Prescribe These Combos?
It’s not because they don’t know the risks. It’s because they’re under pressure. A patient with chronic pain and anxiety might get an opioid for pain and a benzodiazepine for panic. It’s quick. It’s easy. But it’s not safe.
Doctors often lack clear guidance. One study found 69% of hospitalizations for depression involved multiple CNS drugs, yet clinicians had little training on how to weigh the risks. Even when guidelines exist, prescribing habits change slowly. Despite the CDC’s 2016 recommendation against co-prescribing opioids and benzodiazepines, over 10% of chronic opioid users still got both in 2020.

What Can You Do?
If you’re taking more than one CNS depressant, don’t panic-but do act. Here’s how:
- Ask your doctor for a full medication review. Bring every pill, patch, and supplement you take. Include OTC drugs and alcohol use.
- Ask if any meds can be replaced. For anxiety, consider therapy, SSRIs, or non-benzodiazepine options like buspirone. For sleep, try CBT-I instead of sleeping pills.
- Request deprescribing. Slowly reducing or stopping one drug at a time lowers fall risk by 32% and cuts cognitive decline by 27% over a year.
- Use a medication tracker. Apps or printed lists help you spot overlaps. Show them to every provider you see.
- Never drink alcohol with sedatives. Not even one drink. The interaction is unpredictable and dangerous.
Many clinics now use Clinical Decision Support (CDS) tools that flag dangerous combinations before a prescription is written. If your doctor doesn’t use one, ask why. Systems that include the Beers Criteria for seniors have reduced unsafe prescribing by 28%.
The Future Is Safer-If We Push for It
By 2025, most electronic health records will automatically warn doctors about dangerous drug combos. Early pilot programs show this could cut adverse events by up to 35%. Pharmacogenomic testing is also emerging. Some people have gene variants that slow how their bodies break down sedatives. Testing for these could prevent overdoses before they happen.
But technology alone won’t fix this. It takes patients speaking up. It takes doctors listening. It takes systems that prioritize safety over speed.
If you’re on multiple sedatives, your life isn’t just at risk-you’re being treated like a statistic. You deserve better. Ask the questions. Demand alternatives. Your breathing, your mind, and your future depend on it.
Can you die from mixing just two sedatives?
Yes. Even two CNS depressants-like an opioid and a benzodiazepine-can cause fatal respiratory depression. The FDA found this combination increases overdose death risk by 2.5 to 4.5 times compared to opioids alone. It doesn’t take a cocktail of drugs. Just two can be enough.
Is it safe to take a sleeping pill if I’m already on an anti-anxiety med?
No. Most sleep medications like Ambien or Lunesta are CNS depressants, just like Xanax or Valium. Taking them together multiplies sedation, slows breathing, and increases the risk of overdose. Even if they were prescribed by different doctors, the combined effect is dangerous. Always ask your pharmacist or prescriber if your meds interact.
Can alcohol be the only dangerous drug in this mix?
Alcohol is one of the most common and deadly CNS depressants. Even a single drink can dangerously boost the effect of opioids, benzodiazepines, or sleep meds. It doesn’t matter if you’re having a glass of wine at dinner or a beer after work-the interaction is the same. Many overdoses happen because people don’t realize alcohol counts as a sedative.
Are over-the-counter sleep aids safe to use with prescription sedatives?
No. Products like Benadryl, Tylenol PM, or Unisom contain diphenhydramine or doxylamine, which are strong sedatives. Combining them with prescription benzodiazepines or opioids can cause extreme drowsiness, confusion, slowed breathing, and even coma. These OTC drugs are not harmless just because they’re available without a prescription.
What should I do if I think someone is overdosing on sedatives?
Call 911 immediately. Signs include slow or irregular breathing, blue lips or fingertips, unresponsiveness, or snoring/gurgling sounds. If naloxone (Narcan) is available and the person took an opioid, give it. But naloxone won’t reverse benzodiazepine or alcohol overdose. Emergency care is still required. Do not wait to see if they "sleep it off." This is a medical emergency.
Can I just reduce my dose instead of stopping?
Reducing your dose is often safer than stopping suddenly-but only under medical supervision. Suddenly quitting some sedatives, especially benzodiazepines or barbiturates, can cause seizures, hallucinations, or life-threatening withdrawal. Work with your doctor to create a slow, personalized tapering plan. Many people successfully reduce or stop these meds with proper support.





13 Comments