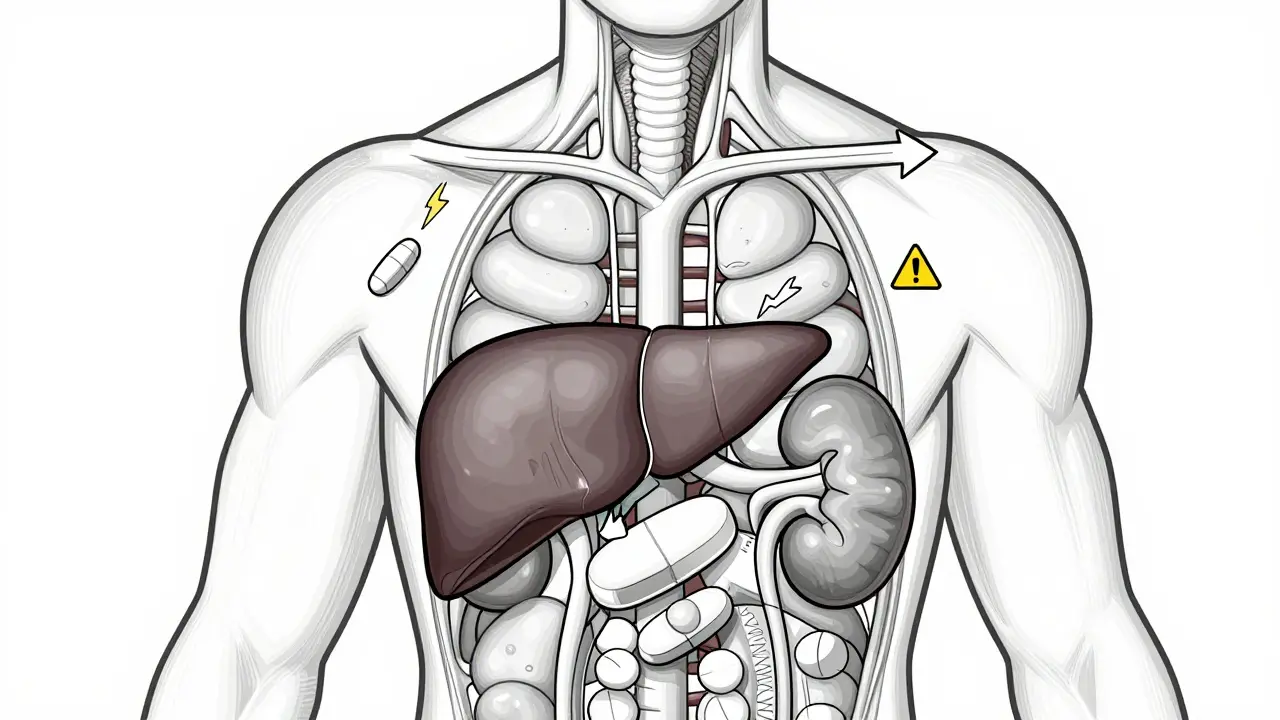
When you take a medication like warfarin, levothyroxine, or tacrolimus, even a tiny change in your dose can mean the difference between healing and harm. These are NTI drugs - Narrow Therapeutic Index drugs. That means the gap between a safe, effective dose and a dangerous one is razor-thin. A 5% increase in blood levels might cause toxicity. A 5% drop could make the drug useless. And here’s the real problem: when you switch from one generic version of an NTI drug to another - even if both are FDA-approved - your body might react differently.
What Makes a Drug an NTI Drug?
Not all medications are created equal. Most drugs have a wide safety margin. You can miss a dose or take it a little late, and nothing serious happens. But NTI drugs? They don’t forgive mistakes. The FDA doesn’t publish an official list, but it’s clear which ones matter: warfarin, lithium, phenytoin, digoxin, cyclosporine, tacrolimus, levothyroxine, and theophylline. These drugs are used for life-threatening or chronic conditions - heart failure, epilepsy, organ transplants, thyroid disorders, blood clots. One wrong move, and you could end up in the hospital.
The FDA requires tighter standards for these drugs. For regular generics, bioequivalence is measured at 80-125% of the brand-name drug’s effect. For NTI drugs? That range shrinks. Some require 90-111%. For others, like tacrolimus, the acceptable variation in blood concentration is as tight as 95-105%. That’s not a typo. It’s half the wiggle room. Why? Because even small differences in how the body absorbs the drug can lead to rejection of a transplanted organ, a seizure, or a dangerous blood clot.
Generic Switching: The Hidden Risk
Here’s where things get messy. You’re on a generic version of levothyroxine. Your pharmacist switches you to another generic - same active ingredient, same FDA approval. Sounds harmless, right? But studies show that switching between different manufacturers of NTI drugs can cause measurable changes in blood levels. One 2019 study found that different generic tacrolimus capsules varied in active ingredient content by as much as 14% - from 86% to 100% of the brand’s level. That’s not a big difference on paper. But for someone who just had a kidney transplant, that shift could trigger rejection.
Real-world data backs this up. A 2015 study of kidney transplant patients found a 21.9% coefficient of variation in tacrolimus blood levels when patients switched between generic brands. That’s high variability - meaning some patients got too much, others too little. In another study, switching between cyclosporine formulations led to a 15.3% higher rate of acute organ rejection. These aren’t rare cases. They’re documented outcomes.
And it’s not just transplant patients. For people on warfarin, switching generics has been linked to a 0.32 increase in INR variability - a measure of blood thinning. That might sound small, but INR needs to stay between 2 and 3. Go above 4, and you risk internal bleeding. Drop below 2, and you risk a stroke. That’s not a range you want to gamble with.
What the FDA Says vs. What Doctors See
The FDA’s official stance is clear: “Generic NTI drugs are therapeutically equivalent.” They approve them based on bioequivalence studies. And statistically, most studies show no major difference between brand and generic, or even between different generics. A 2021 FDA analysis of levothyroxine found no meaningful difference in TSH levels between brand-name Synthroid and generics. The mean difference? 0.03 mIU/L. Statistically insignificant.
But here’s the disconnect: doctors and patients don’t always see it that way. A 2019 survey found that 63% of pharmacists had received complaints from patients or doctors after switching NTI generics. Epilepsy patients reported breakthrough seizures after switching antiepileptic generics. Thyroid patients said they felt “off” - tired, anxious, weight changes - even when lab numbers looked fine. These aren’t just placebo effects. They’re real experiences.
The American Academy of Neurology, the Epilepsy Foundation, and other specialty groups have issued guidelines advising against automatic substitution of NTI antiepileptic drugs. Why? Because population-level data doesn’t capture individual sensitivity. One person’s body might absorb one generic perfectly. The next person’s body might not. And if you’re switching manufacturers every few months - because insurance changes, pharmacy stock runs out, or cost-cutting policies kick in - your body never settles.

Why Do These Differences Even Happen?
It’s not about the active ingredient. That’s the same. The problem lies in the fillers, coatings, and manufacturing processes. A different binder in a pill might slow down how fast the drug dissolves. A different coating might change how it’s absorbed in the gut. These aren’t just “inactive” ingredients - they’re critical to how the drug behaves in your body. For NTI drugs, even minor changes in dissolution rate can throw off blood levels.
Brand-name manufacturers often spend years perfecting their formulation. Generic makers? They just need to match the FDA’s bioequivalence range. And while most do, some don’t. That’s why the FDA now requires additional in vivo testing for drugs like tacrolimus - because lab tests alone can’t predict how the drug will behave in a living person.
What You Can Do
If you’re on an NTI drug, here’s what you need to know:
- Know your drug. Is it on the NTI list? Warfarin? Levothyroxine? Lithium? Tacrolimus? If yes, treat it differently.
- Ask your pharmacist. When you refill, ask if the manufacturer changed. Don’t assume it’s the same.
- Request a specific brand or generic. You have the right to ask for the version that works for you. Some pharmacies will honor it. Others won’t - but it’s worth asking.
- Monitor closely. If you switch, get your blood levels checked within 2-4 weeks. For warfarin, that’s INR. For levothyroxine, it’s TSH. For tacrolimus, it’s trough levels. Don’t wait for symptoms.
- Speak up. If you feel different after a switch - even if labs look fine - tell your doctor. Your experience matters.
State Laws Are Changing - But Slowly
As of 2022, 27 U.S. states have laws restricting automatic substitution of NTI drugs. Some require the prescriber to write “Do Not Substitute.” Others require pharmacists to notify the prescriber before switching. But many states still allow automatic substitution - even for drugs like phenytoin and carbamazepine, where seizure control is fragile.
Pharmacists in states with strict laws are far less likely to switch NTI generics without permission. In states without laws? It happens all the time. And insurance companies? They push for the cheapest option - even if it’s not the safest one for you.
The Bottom Line
Yes, the FDA says generics are safe. And for most drugs, they are. But NTI drugs aren’t most drugs. They’re the ones that demand precision. Switching between manufacturers might be fine for your ibuprofen. It’s not fine for your transplant medication or your seizure control.
Don’t let cost-cutting policies override your health. If you’re on an NTI drug, treat it like a precision instrument - not a commodity. Stay informed. Stay vigilant. And never assume that “same drug” means “same effect.” Your body knows the difference. So should your care team.
Are all generic drugs the same, even for NTI medications?
No. While all FDA-approved generics must contain the same active ingredient and meet bioequivalence standards, NTI drugs have stricter limits. Even small differences in inactive ingredients or manufacturing can affect how the drug is absorbed. For drugs like tacrolimus or warfarin, switching between generic brands can lead to measurable changes in blood levels - even if both are technically "equivalent."
Can I ask my pharmacist not to switch my NTI drug?
Yes. You have the right to request a specific brand or generic manufacturer. Some pharmacies will honor this request, especially if your doctor writes "Do Not Substitute" on the prescription. If they refuse, ask to speak with the pharmacist-in-charge. In some states, laws require them to notify your prescriber before switching NTI drugs.
How do I know if my NTI drug has been switched?
Check the pill’s imprint, color, or shape - it may look different. Look at the pharmacy label - it should list the manufacturer’s name. If you’re unsure, ask the pharmacist. They’re required to tell you if the generic has changed. Don’t rely on memory. Keep a record of which manufacturer you’re on.
What should I do if I feel worse after switching generics?
Don’t ignore it. Contact your doctor immediately. Get your blood levels tested - INR for warfarin, TSH for levothyroxine, trough levels for tacrolimus. Even if your symptoms seem mild, they could signal a dangerous shift. Keep a journal of how you feel before and after each switch. That data helps your doctor make better decisions.
Is there a list of NTI drugs I can check?
The FDA doesn’t publish one official list, but key NTI drugs include warfarin, levothyroxine, lithium, phenytoin, carbamazepine, digoxin, cyclosporine, tacrolimus, and theophylline. Your doctor or pharmacist can confirm if your medication is on this list. You can also check the FDA’s product-specific bioequivalence guidance documents for each drug.








9 Comments