Aromatase Inhibitor Selector
Use this tool to compare different aromatase inhibitors and select the most suitable one based on your specific needs.
When it comes to lowering estrogen levels-whether for breast cancer treatment, off‑label testosterone therapy, or managing estrogen‑related side effects-Arimidex is often the first name that pops up. But it’s not the only option on the market. This guide breaks down how Arimidex stacks up against its main competitors, natural alternatives, and when each might be the better pick.
TL;DR
- Arimidex (Anastrozole) is a non‑steroidal aromatase inhibitor (AI) used mainly in post‑menopausal breast cancer.
- Letrozole is slightly more potent but carries a higher risk of joint pain.
- Exemestane is a steroidal AI that can be easier on bone density.
- Tamoxifen works differently (as a selective estrogen receptor modulator) and is not a true AI.
- Natural options like soy isoflavones may help mildly, but they aren’t substitutes for prescription AIs.
What is Arimidex (Anastrozole)?
Arimidex is a potent, non‑steroidal aromatase inhibitor that blocks the enzyme aromatase from converting androgens into estrogen. It was approved by the FDA in 1995 for treating hormone‑receptor‑positive breast cancer in post‑menopausal women. Typical dosing is 1mg daily, taken with or without food.
Because it reduces circulating estradiol by up to 97%, Arimidex can also be prescribed off‑label to curb estrogen‑related side effects in men on testosterone replacement therapy (TRT). Common side effects include hot flashes, joint stiffness, and a modest decrease in bone mineral density.
Key Alternatives to Consider
When doctors talk about “alternatives,” they usually mean other aromatase inhibitors or drugs that affect estrogen pathways in a different way.
- Letrozole - a non‑steroidal AI that’s slightly more potent than Arimidex.
- Exemestane - a steroidal AI, sometimes called a “suicide inhibitor” because it permanently deactivates the aromatase enzyme.
- Tamoxifen - a selective estrogen receptor modulator (SERM) that blocks estrogen receptors rather than lowering estrogen levels.
- Natural options - soy isoflavones, flaxseed, and certain berry extracts that have mild aromatase‑inhibiting properties.
How Do They Differ? A Quick Comparison
| Attribute | Arimidex (Anastrozole) | Letrozole | Exemestane | Tamoxifen (SERM) | Natural (Soy Isoflavones) |
|---|---|---|---|---|---|
| Drug class | Non‑steroidal AI | Non‑steroidal AI | Steroidal AI | SERM | Phyto‑estrogen |
| Typical dose | 1mg daily | 2.5mg daily | 25mg daily | 20mg twice daily | 30‑50g soy protein/day |
| Estrogen reduction | ~97% | ~98% | ~95‑96% | ~0% (blocks receptors) | ~10‑20% (mild) |
| Common side effects | Hot flashes, joint pain, mild bone loss | Joint pain, fatigue, higher risk of osteoporosis | Hot flashes, possible liver enzyme elevation | Vaginal discharge, risk of blood clots | GI discomfort, possible thyroid impact |
| Cost (US, per month) | $30‑$45 (generic) | $45‑$60 | $50‑$70 | $25‑$35 | Varies (food‑based) |
| Best for | Post‑menopausal breast cancer, TRT‑related estrogen control | Patients needing stronger estrogen suppression | Those with bone‑density concerns | Pre‑menopausal patients, breast‑cancer prevention | People seeking mild, dietary support |
When Might You Choose Letrozole?
Letrozole’s 2.5mg daily dose can shave off a few extra points of estrogen compared with Arimidex. In clinical trials for advanced breast cancer, it showed a slightly longer progression‑free survival. However, that extra potency often comes with stiffer joint aches and a higher chance of bone density loss. If you’re already dealing with osteoporosis or have a history of fractures, Letrozole may not be the safest bet.

When Is Exemestane a Better Fit?
Exemestane’s steroidal structure means it binds irreversibly to aromatase, essentially “shutting down” the enzyme for the life of that protein molecule. This can be advantageous for patients who have developed resistance to non‑steroidal AIs. Moreover, because it mimics some androgen activity, it may have a milder impact on bone health-making it a popular switch option after long‑term Arimidex use.
Why Some Doctors Still Prescribe Tamoxifen
Unlike AIs, Tamoxifen doesn’t lower estrogen; it blocks the hormone at its receptor sites. That makes it useful for pre‑menopausal women whose ovaries are still pumping out estrogen-AIs would be ineffective until menopause. Tamoxifen also carries a protective effect against certain types of uterine cancer but raises the risk of deep‑vein thrombosis, so the risk profile is quite different.
Can Natural Alternatives Replace Prescription AIs?
Phyto‑estrogens such as soy isoflavones do exhibit modest aromatase‑inhibiting activity in lab studies. In practice, they may lower estradiol by 10‑20% at best, which is nowhere near the 95‑+% suppression offered by prescription AIs. For someone looking for a gentle, diet‑based approach, they can be a nice adjunct, but relying on them alone for breast‑cancer treatment would be unsafe.
Deciding Factors: How to Pick the Right Option
- Stage of disease or purpose: Early‑stage breast cancer vs. TRT‑related estrogen control.
- Bone health: If you have osteopenia, Exemestane may be kinder to your skeleton.
- Side‑effect tolerance: Letrozole’s joint pain vs. Tamoxifen’s clot risk.
- Cost and insurance coverage: Generic Arimidex is often the cheapest.
- Age and menopausal status: Pre‑menopausal women usually get Tamoxifen.
Discuss these points with your oncologist or endocrinologist. They can run baseline bone density scans, liver function tests, and lipid panels to gauge which drug poses the least overall risk for you.
Practical Tips for Managing Side Effects
- Take a calcium‑vitaminD supplement (1,000mg calcium + 800IU vitaminD) to protect bone density.
- Schedule low‑impact exercise (swimming, walking) 3‑4 times a week to keep joints mobile.
- Stay hydrated; hot flashes often worsen with dehydration.
- If joint pain becomes severe, ask about a short‑term NSAID or switching to Exemestane.
- Consider a bisphosphonate (e.g., alendronate) if bone loss is documented.
Frequently Asked Questions
Can I take Arimidex for weight loss?
No. Arimidex is designed to lower estrogen, not to burn fat. Some people misuse it hoping to reduce water retention, but there’s no solid evidence it aids weight loss and it can cause serious side effects.
How long can I stay on an aromatase inhibitor?
Duration depends on the indication. In breast‑cancer adjuvant therapy, doctors often prescribe 5‑10years. For TRT‑related estrogen control, treatment may be ongoing but requires regular monitoring of bone density and liver enzymes.
Is it safe to switch from Arimidex to Letrozole?
Switching is common when a patient develops resistance or intolerable side effects. Because both are non‑steroidal AIs, the transition is straightforward-just follow your doctor’s dosing schedule and monitor blood work.
Do natural supplements work as well as prescription AIs?
Natural supplements can provide a mild reduction in estrogen, but they fall far short of the 95‑plus% suppression achieved by prescription AIs. They’re best used as complementary, not as primary therapy.
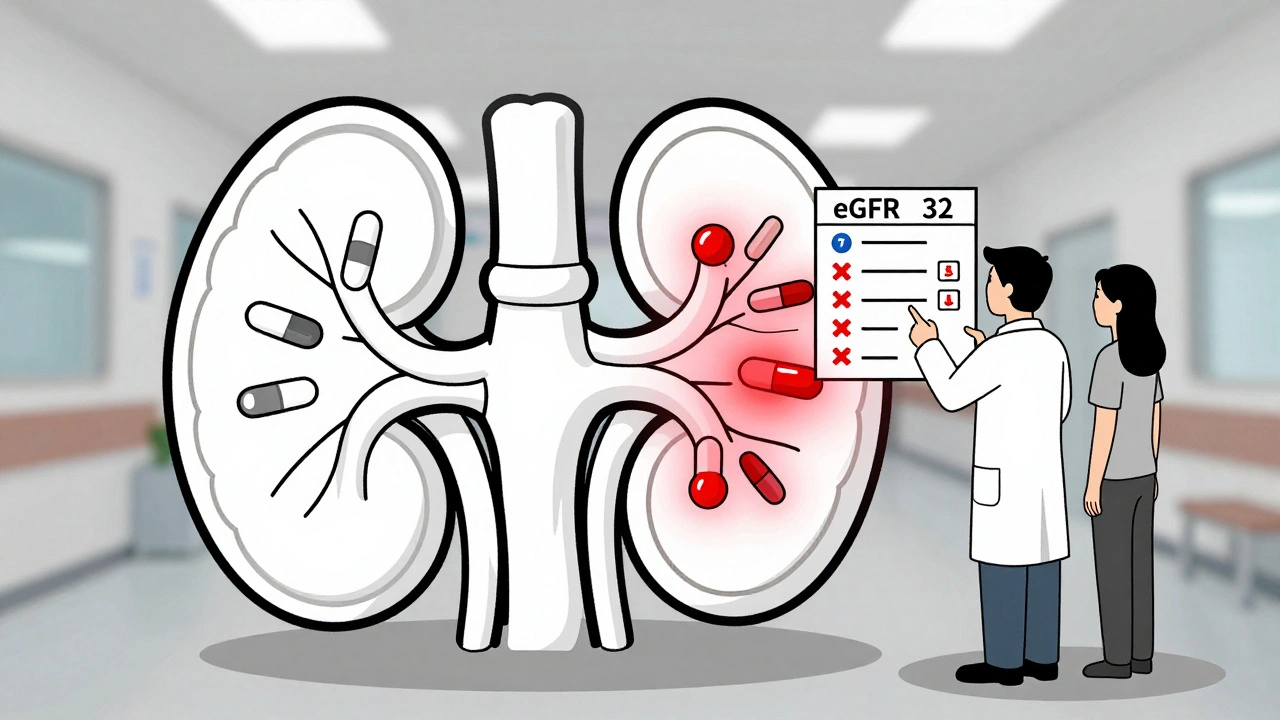
What should I monitor while on an AI?
Key labs include estradiol levels, liver function tests, lipid profile, and bone mineral density scans every 1‑2years. Keep an eye on joint pain, hot flashes, and any new mood changes.
Bottom line: Arimidex remains a solid first‑line choice for most post‑menopausal patients needing strong estrogen suppression. Letrozole offers a bit more potency at the cost of joint discomfort, Exemestane may spare bone health, and Tamoxifen works best when you need receptor blockade instead of hormone lowering. Natural foods can supplement the plan but shouldn’t replace a prescription AI. Talk to your healthcare provider, weigh the side‑effect profile, and pick the option that aligns with your health goals.







10 Comments