Antiplatelet Therapy Calculator
Loading: 60 mg
Loading: 300-600 mg
Loading: 180 mg
(Lower risk = better efficacy)
(Lower risk = safer)
When doctors need to stop a blood clot from forming after a heart attack or stent placement, they often turn to Prasugrel is a third‑generation P2Y12 inhibitor that blocks platelet activation more powerfully than older drugs. But is it always the right choice? Below we break down how Prasugrel stacks up against the most common alternatives - clopidogrel, ticagrelor and aspirin - so you can see where each one shines and where it falls short.
What is Prasugrel?
Prasugrel (brand name Effient) was approved by the FDA in 2009 for use in acute coronary syndrome (ACS) patients who undergo percutaneous coronary intervention (PCI). It belongs to the thienopyridine class, which also includes clopidogrel.
How Prasugrel Works - the Mechanism
The drug binds irreversibly to the P2Y12 receptor on platelet surfaces, preventing ADP from triggering the clotting cascade. Because it’s a pro‑drug, it’s metabolised by liver enzymes - mainly CYP2C19 and CYP3A4 - into its active form. This rapid conversion gives Prasugrel a faster onset (about 30 minutes) compared with clopidogrel’s 2‑4 hour lag.
Key Alternatives
- Clopidogrel (Plavix) - the first‑generation thienopyridine, often used for long‑term secondary prevention.
- Ticagrelor (Brilinta) - a reversible, non‑thienopyridine P2Y12 antagonist that works without metabolic activation.
- Aspirin - an irreversible cyclo‑oxygenase (COX‑1) inhibitor that reduces thromboxane A2 formation; usually combined with a P2Y12 blocker in dual antiplatelet therapy (DAPT).
Efficacy: Clinical Trial Snapshot
Three landmark trials give us the most reliable numbers:
- TRITON‑TIMI 38: Compared Prasugrel with clopidogrel in 13,500 ACS patients undergoing PCI. The primary endpoint (death, myocardial infarction or stroke) fell from 9.4% to 6.8% (relative risk reduction 22%).
- PLATO: Bench‑marked ticagrelor against clopidogrel in 18,000 ACS patients. Ticagrelor cut the composite endpoint to 9.8% vs 11.7% for clopidogrel (RRR 16%).
- CAPRIE: Older study showing clopidogrel’s modest 8.7% vs aspirin’s 11.2% for the same endpoint.
In head‑to‑head meta‑analyses, Prasugrel’s absolute risk reduction is roughly 1-2% better than ticagrelor for preventing stent thrombosis, but the gap narrows when both are used in DAPT with aspirin.
Safety and Bleeding Risk
Bleeding is the trade‑off for stronger platelet inhibition. The TRITON‑TIMI 38 trial reported major bleeding in 2.9% of Prasugrel patients versus 1.8% on clopidogrel. Ticagrelor’s major bleeding rate sat at 2.3% in PLATO. Aspirin adds about a 0.5% incremental risk when combined with any P2Y12 inhibitor.
Specific safety concerns:
- Prasugrel is contraindicated in patients with a history of stroke or transient ischemic attack (TIA) - the bleeding risk jumps dramatically.
- Ticagrelor can cause dyspnoea in up to 14% of users, likely due to adenosine reuptake inhibition.
- Clopidogrel’s effectiveness is reduced in patients who are poor metabolizers of CYP2C19 (about 15% of Asian populations).
Dosing and Administration
| Drug | Loading Dose | Maintenance Dose | Renal Adjustments |
|---|---|---|---|
| Prasugrel | 60 mg orally | 10 mg daily | Reduce to 5 mg if age ≥75 yr or weight <60 kg |
| Clopidogrel | 300-600 mg orally | 75 mg daily | No adjustment needed |
| Ticagrelor | 180 mg (two 90 mg tablets) | 90 mg twice daily | Avoid in severe hepatic impairment |
| Aspirin | 162‑325 mg (chewed) | 81 mg daily | Reduce in CKD stages 4‑5 |
All three P2Y12 inhibitors are taken with food to improve absorption, but ticagrelor must be taken twice daily, which can affect adherence.
Cost and Accessibility (2025 US market)
Pricing can sway the final decision:
- Prasugrel: approx. $12‑$15 per tablet (generic available since 2023).
- Clopidogrel: $0.30‑$0.60 per tablet (widely generic).
- Ticagrelor: $7‑$9 per tablet (brand‑only, no generic yet).
- Aspirin: <$0.05 per tablet.
Insurance formularies usually place clopidogrel on a lower tier, making it the most budget‑friendly option for long‑term therapy.
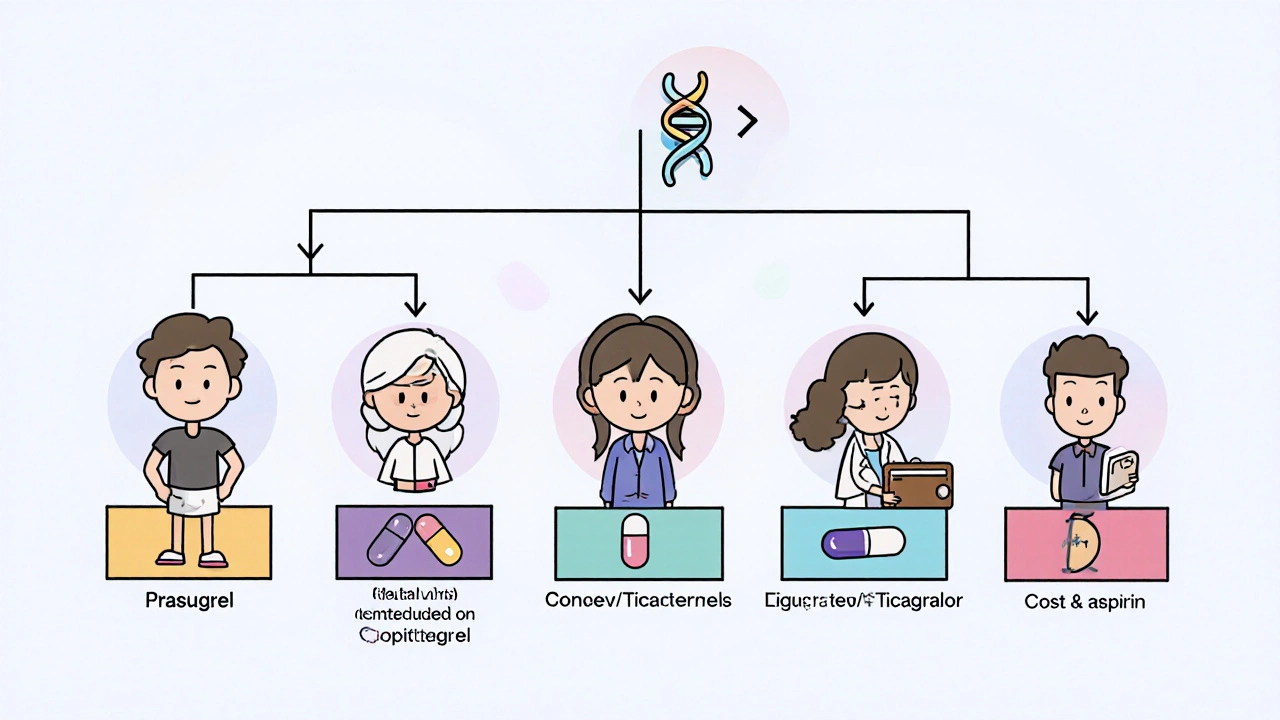
Best‑Fit Scenarios - Who Should Choose What?
| Patient Profile | Preferred Agent | Why? |
|---|---|---|
| Young (<65 yr), high thrombotic risk, no bleeding history | Prasugrel | Highest platelet inhibition, lower recurrent MI |
| Elderly (≥75 yr) or low body weight (<60 kg) | Clopidogrel (or reduced‑dose Prasugrel) | Lower bleeding risk |
| History of stroke/TIA | Clopidogrel or Ticagrelor | Prasugrel contraindicated |
| Patients with CYP2C19 poor‑metabolizer genotype | Ticagrelor | Works without metabolic activation |
| Cost‑sensitive, long‑term secondary prevention | Clopidogrel + aspirin | Effective, cheap, generic |
| Patients experiencing dyspnoea on ticagrelor | Prasugrel or Clopidogrel | Avoids ticagrelor’s side‑effect |
Bottom Line
If you need the most aggressive platelet block after a high‑risk PCI and you’re under 75 years old with a weight above 60 kg, Prasugrel often gives the best protection against repeat heart attacks. For older patients, those with a stroke history, or anyone worried about bleeding, clopidogrel remains a safe, inexpensive fallback. Ticagrelor sits in the middle - a strong alternative when genetic testing shows clopidogrel won’t work, but the twice‑daily dosing and dyspnoea risk can be limiting.
Frequently Asked Questions
Can I switch from clopidogrel to prasugrel after starting treatment?
Yes, but doctors usually wait at least 5 days after stopping clopidogrel (or 24 hours if you’ve been on a loading dose) before loading prasugrel to avoid overlapping antiplatelet effect.
Is there a generic version of prasugrel?
Generic prasugrel entered the U.S. market in 2023 and is now stocked by most major pharmacies. The generic matches the brand in dose and efficacy.
What lab test predicts clopidogrel response?
A CYP2C19 genetic panel identifies poor metabolizers who may have reduced activation of clopidogrel, guiding clinicians toward ticagrelor or prasugrel.
Why is prasugrel contraindicated after a stroke?
Patients with prior cerebrovascular events already have a higher baseline risk of intracranial bleeding. Prasugrel’s potency magnifies that risk, so guidelines advise against its use.
Does aspirin still add value when using a P2Y12 inhibitor?
Yes. Dual antiplatelet therapy (DAPT) with aspirin plus a P2Y12 blocker reduces early stent thrombosis more than either agent alone. Guidelines usually recommend DAPT for 6‑12 months after PCI.








11 Comments