REMS Complexity Calculator
How complex is your REMS program?
Estimate the time and administrative burden of REMS requirements for high-risk medications. This tool helps healthcare providers understand the practical impact of FDA risk management requirements on patient care.
When a drug is powerful enough to save lives, it’s often powerful enough to kill too. That’s the tightrope the FDA walks every day. For some medications-especially those used in cancer, severe mental illness, or chronic autoimmune conditions-the risks are too high to just slap on a warning label and call it done. Enter REMS: Risk Evaluation and Mitigation Strategies. These aren’t suggestions. They’re legally binding rules. But do they actually make patients safer? Or are they just bureaucratic hurdles that slow down care?
What REMS Really Is (And What It’s Not)
REMS isn’t just another patient handout. It’s a full system-engineered by the FDA after the 2007 Food and Drug Administration Amendments Act-to keep dangerous drugs on the market without letting patients get hurt. Think of it as a safety net woven into the prescription process itself. Before REMS, the FDA used voluntary RiskMAPs. They didn’t work. Compliance? As low as 35%. After REMS launched in 2008, mandatory components pushed compliance to 75-95%.
There are three core parts to REMS. First, Medication Guides-printed, FDA-approved instructions patients must receive with every fill. Forty-five REMS programs require this. Second, Communication Plans-letters or training sessions sent to doctors to make sure they understand the dangers. Third, and most intense, Elements to Assure Safe Use (ETASU). These are the heavy lifters. They force prescribers to get certified, pharmacies to have emergency equipment on hand, and clinics to monitor patients for hours after treatment.
Take Zyprexa Relprevv, a shot for schizophrenia. Because 0.8% of patients suffer sudden confusion and sedation after injection, the REMS requires every clinic to watch the patient for three full hours. No exceptions. No shortcuts. That’s not a recommendation. That’s the law.
Who Uses REMS? The Real Numbers
Out of nearly 20,000 drugs on the U.S. market, only 150 are covered by REMS. That’s less than 1%. But those 150 drugs? They account for $120 billion in annual sales. That’s not a coincidence. REMS isn’t for common pills like statins or antibiotics. It’s for the high-stakes, high-risk drugs that can’t be pulled from shelves but can’t be left uncontrolled either.
The biggest users? Oncology. Nearly 40% of all REMS programs target cancer drugs. Neurology comes next-19%-for drugs like Tysabri, used in multiple sclerosis. Immunology follows. These are conditions where one wrong step can mean death. Tysabri’s REMS, for example, demands a JC virus antibody test before every infusion. Why? Because without it, patients face a rare but deadly brain infection. Clinics that followed this rule saw a 30% drop in serious side effects.
But here’s the twist: REMS isn’t just about saving lives. It’s also about getting drugs approved. Between 2018 and 2022, 12 new drugs reached patients only because a REMS plan made them acceptable to the FDA. Without it, they’d have been rejected.
The Cost of Safety: Time, Money, and Frustration
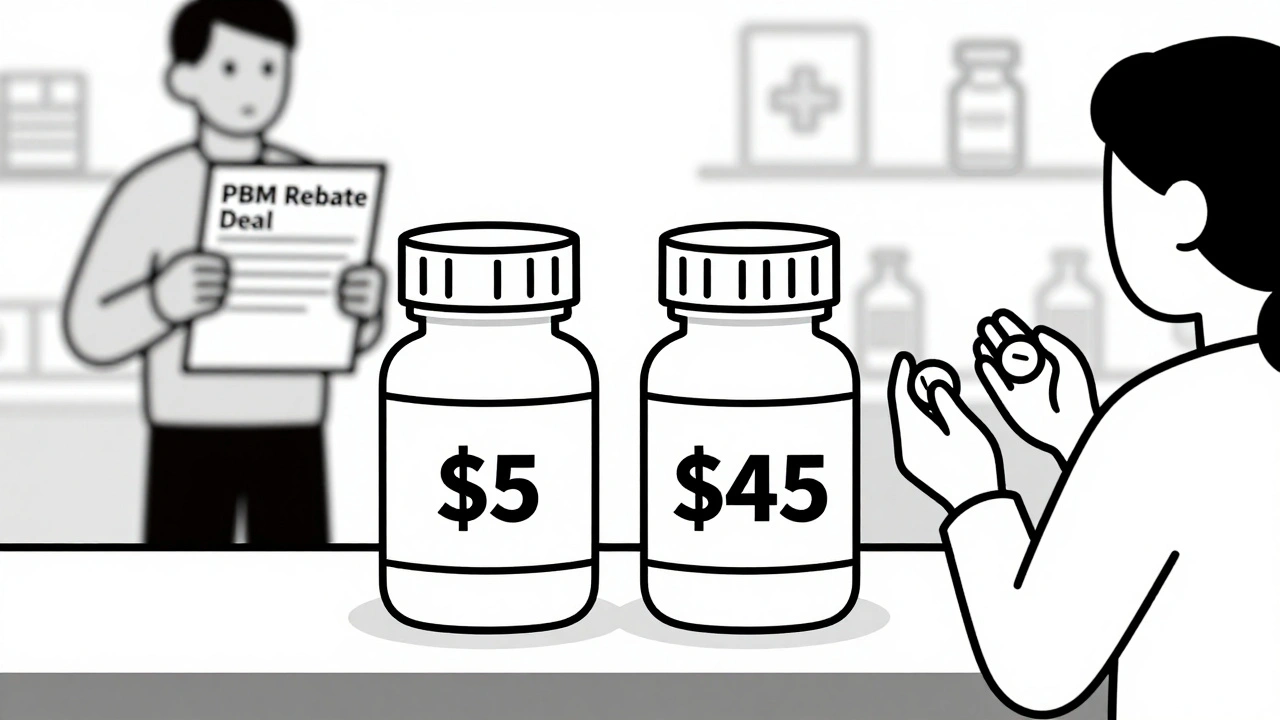
REMS doesn’t come cheap. For manufacturers, the first year of setting up a complex REMS can cost over $18 million. After that? $5.3 million a year, just to keep it running. That’s not just paperwork. It’s staff, portals, training, audits, and compliance officers.
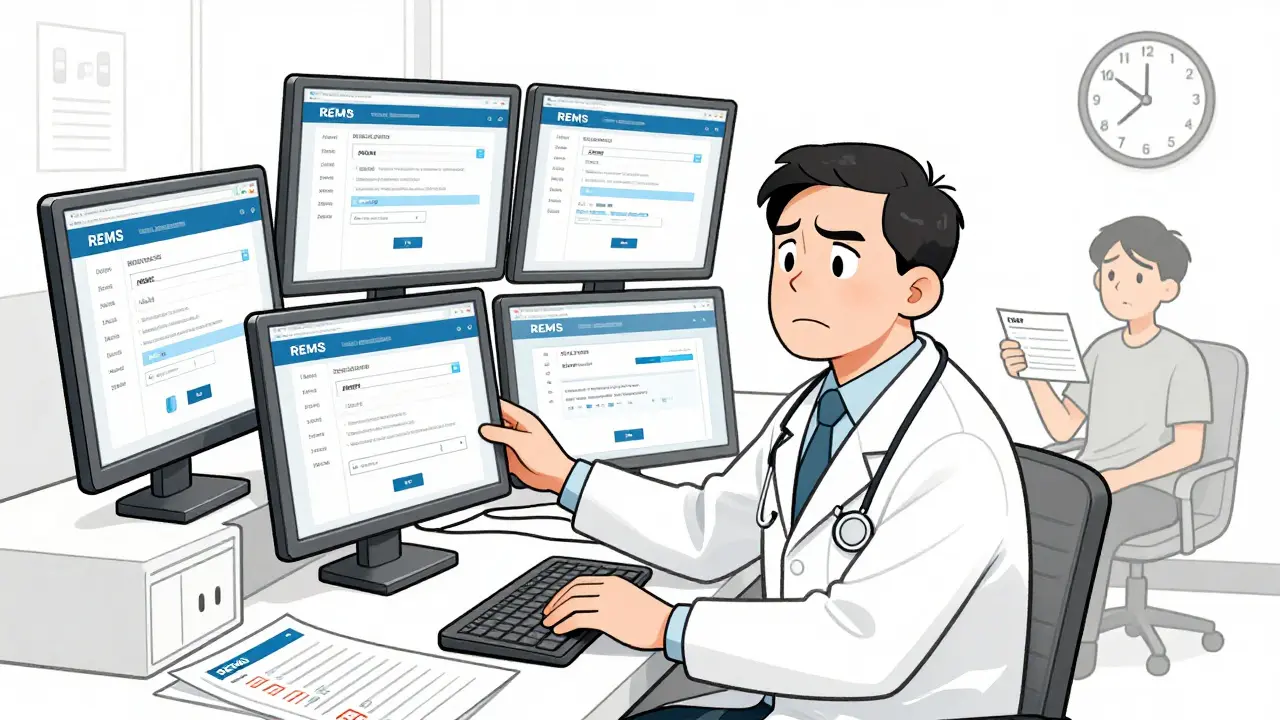
For doctors? It’s a nightmare. A 2022 survey of 1,200 physicians found 68% said REMS caused delays in treatment. Oncologists? 82%. Neurologists? 76%. Nearly half admitted they’d skipped prescribing a drug because the REMS process was too messy. One doctor told me (anonymously) he gave up on prescribing a life-saving leukemia drug because it required five separate registrations across three different websites. He didn’t have time.
Pharmacists are drowning too. A 2022 survey found 57% of REMS-required medications needed three or more registrations. Each one took an average of 4.2 hours to set up per patient. That’s not just inconvenient-it’s dangerous. Patients waiting days for a prescription can miss critical treatment windows.
Do REMS Actually Change Outcomes? The Evidence Gap
This is the big question. Do these rules make people live longer? Have fewer strokes? Survive cancer better?
The FDA’s own 2020 report admitted: only 30% of REMS programs had enough data to answer that. The rest? They track things like: “Did the patient get the guide?” “Did the doctor complete the training?” “Was the observation logged?”
That’s process, not outcome. It’s like measuring whether a firefighter showed up to the fire-not whether the house was saved.
Dr. Peter Lurie, a former FDA official, put it bluntly: “The evidence for REMS changing clinical outcomes remains thin.” He’s not alone. Industry groups argue REMS adds cost without proof of benefit. But here’s the counter: when outcomes are measured, they improve. The Tysabri example isn’t an outlier. A study of a REMS program for a rare blood disorder showed a 40% drop in life-threatening reactions after mandatory provider training was enforced.
The problem isn’t that REMS doesn’t work. It’s that we’re not measuring the right things.
The Future: From Checkboxes to Clinical Results
The FDA knows this. In 2023, they released draft guidance saying: by 2025, new REMS programs must prove they’re improving actual patient outcomes-not just ticking boxes. That’s a seismic shift.
They’re also building tools to make REMS less painful. The REMS@FDA portal now handles 63% of all programs in one place. Before, doctors jumped between five different websites. Now? It’s down to two. And by 2026, 90% of REMS programs will connect directly to electronic health records. That means automatic alerts, no manual forms, no lost paperwork.
There’s even talk of “REMS Lite”-a simplified version for drugs with lower risks. Imagine a medication that needs a warning and a quick online quiz for doctors, but no three-hour observation. That could bring REMS to 50-75 more drugs without overwhelming the system.
By 2028, Deloitte predicts 75% of new REMS programs will require direct clinical outcome data. That’s not just regulation anymore. That’s precision safety.

So, Do REMS and Guides Change Outcomes?
Yes-but not always, and not yet everywhere.
REMS has done what no voluntary system could: make safety mandatory. It’s kept deadly drugs from being pulled, while giving doctors the tools to use them carefully. It’s saved lives in cancer, MS, and psychiatric care. But it’s also created bottlenecks that hurt patients who need help now.
The real win isn’t in the number of guides distributed or the hours of training completed. It’s in fewer ER visits, fewer deaths, fewer treatment delays. The FDA is finally starting to measure that. And when they do, REMS won’t just be a compliance tool. It’ll be a life-saving one.
The question isn’t whether REMS works. It’s whether we’re ready to make it work better.
Are Medication Guides the same as REMS?
No. Medication Guides are just one part of REMS. All REMS programs include patient information, but not all patient guides are part of REMS. Over 2,000 drugs have standard Medication Guides just for general warnings. REMS applies only to drugs with serious, preventable risks-and includes enforceable requirements like provider training, pharmacy certification, or patient monitoring.
Can patients opt out of REMS requirements?
No. REMS requirements are legally mandatory for providers and pharmacies. If a drug requires a certified prescriber or a three-hour observation, those steps can’t be skipped-even if the patient refuses. The goal is to prevent harm before it happens. Skipping steps puts both the patient and the provider at legal and clinical risk.
Why are REMS programs so common in cancer treatment?
Cancer drugs are often extremely powerful, with narrow windows between effectiveness and toxicity. Many cause severe immune reactions, organ damage, or fatal infections. REMS ensures that only trained providers prescribe them, pharmacies handle them safely, and patients are monitored for early signs of danger. Of the 72 active REMS programs, 29 (40%) are for cancer drugs-more than any other category.
How long does it take to get certified for a REMS program?
It varies. For simple REMS with just a Medication Guide, providers may need 15-30 minutes of training. For ETASU programs-like those for opioids or certain cancer drugs-it can take 8 to 16 hours of certified training. Some require annual recertification. The process is designed to be thorough, but fragmented portals make it slower than it should be.
Is REMS used outside the United States?
The U.S. FDA’s REMS is unique in its structure and enforcement. Other countries have risk management plans, but none are as standardized, legally binding, or tied to market approval like REMS. The European Medicines Agency uses Risk Management Plans (RMPs), but they’re less prescriptive and not tied to mandatory certification or monitoring. REMS is a distinctly American regulatory tool.
What’s the biggest challenge with REMS today?
Fragmentation. Prescribers still juggle multiple portals, inconsistent documentation, and delayed approvals. Even with REMS@FDA, many programs remain separate. The biggest barrier isn’t the rules-it’s the infrastructure. Until all REMS programs are fully integrated into electronic health records, delays and errors will persist.
What Comes Next?
REMS is evolving from a compliance checklist into a real-time safety network. By 2026, most programs will auto-populate in your EHR. By 2028, you’ll see data on how many patients avoided hospitalization because of REMS protocols-not just how many got their guides.
The goal isn’t to slow down care. It’s to make sure the right care gets to the right patient, safely and without delay. The tools are getting smarter. The data is getting better. The question now isn’t whether REMS works. It’s whether we’ll let it work as well as it can.







9 Comments