DVT Risk Assessment Calculator
Travel Safety Risk Assessment
Answer these questions to determine your risk level for developing blood clots during international travel.
Your Travel Safety Assessment
Your DVT Risk Level
Travel Safety Recommendations
Traveling on Blood Thinners? Here’s What Actually Works to Prevent Clots
You’re packing your bags for a long-haul flight to Europe. You’ve got your passport, your camera, your favorite snacks. But you’re also on blood thinners-warfarin, rivaroxaban, apixaban, or something else. And now you’re wondering: is this safe? Can you even fly without risking a clot? The truth is, millions of people travel internationally every year while on anticoagulants. Most do it without a problem. But skipping the right prep steps? That’s where things go wrong.
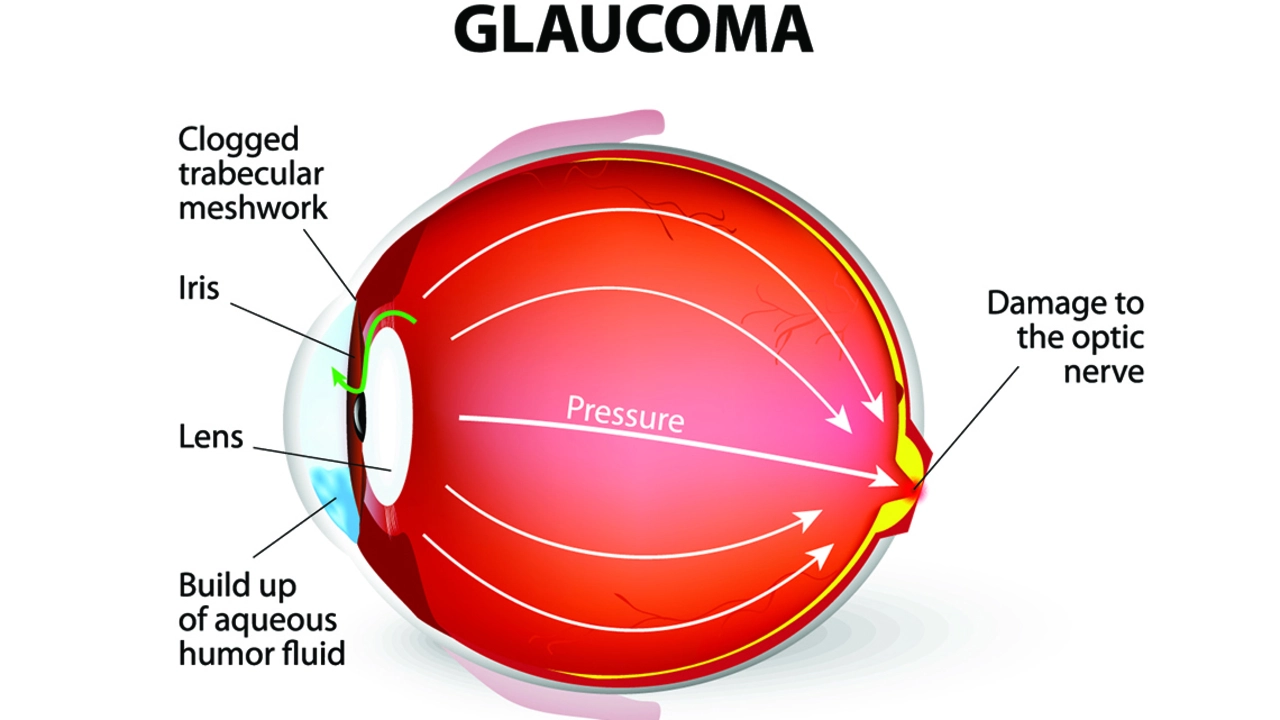
The real danger isn’t the flight itself. It’s sitting still for hours. Immobility slows blood flow, especially in your legs. That’s when clots form-deep vein thrombosis, or DVT. And if that clot breaks loose? It can travel to your lungs and cause a pulmonary embolism. That’s life-threatening. But here’s the good news: you don’t need to cancel your trip. You just need to know what to do.
Who’s at Highest Risk During Travel?
Not everyone on blood thinners needs extra precautions. But if you have any of these, your risk jumps:
- You’re over 40-risk goes up 10% for every decade after 40
- Your BMI is 30 or higher
- You had surgery or a serious injury in the last 3 months
- You’ve had a blood clot before-even years ago
- You have cancer, heart failure, or COPD
- You’re pregnant or within 3 months of giving birth
- You’re on estrogen pills or hormone therapy
- You have a family history of clots or inherited clotting disorders like Factor V Leiden
If you have even one of these, you’re not just a “regular” traveler. You’re high-risk. And that changes your plan. The CDC calls this “risk stratification.” It’s not jargon-it’s your safety checklist.
Don’t Skip Your Medication-Even When Time Zones Change
This is the #1 mistake people make. You land in Tokyo. It’s 3 a.m. your usual pill time. You think: “I’ll take it tomorrow morning.” Big mistake.
Anticoagulants don’t work if you miss doses. Warfarin users especially need steady levels. Skipping even one day can make your blood clot faster than if you’d never taken it. That’s not a myth. It’s what Dr. Susan Coogan at UT Physicians says: “If you skip doses, your blood can actually become MORE sticky.”
Here’s how to handle time zones:
- For warfarin: Take your dose at the same clock time, not the same circadian time. If you usually take it at 7 p.m. Sydney time, and you fly to New York (14-hour difference), take it at 7 p.m. New York time-not 7 a.m. your body thinks it is.
- For DOACs (rivaroxaban, apixaban, etc.): These are more forgiving, but still take them at the same time each day relative to your new time zone.
- Always carry extra pills-enough for 10 days beyond your trip in case of delays.
And if you’re on warfarin? Get your INR checked 1-2 weeks before you leave. Target range? Usually 2.0-3.0 for atrial fibrillation, 2.5-3.5 for mechanical heart valves. If your INR’s too high, you risk bleeding. Too low? You risk clots. Don’t wing it.
Compression Stockings: Not Just for Flight Attendants
You’ve seen them-those tight, knee-high socks travelers wear. They’re not fashion. They’re medical gear.
Graduated compression stockings (GCS) that provide 15-30 mmHg pressure at the ankle are recommended by the American College of Chest Physicians for high-risk travelers. They squeeze your legs just enough to keep blood moving. No magic. Just physics.
Don’t buy random “compression socks” off Amazon. Look for “medical-grade,” “15-30 mmHg,” and “below-knee.” Wear them for the entire flight, even if it’s only 3 hours. Put them on before you leave for the airport.
And here’s a pro tip: if you’re flying economy, pick an aisle seat. It’s not about legroom-it’s about being able to get up and walk every 2-3 hours. Window seats are traps.
Move. Even When You Don’t Feel Like It
Standing up and walking every 2-3 hours is the single most effective non-medication way to prevent DVT. But you’re tired. You’ve got a movie playing. You’re waiting for the meal cart. You think: “I’ll do it later.”
Later doesn’t work.
Do this instead:
- Set a timer on your phone for every 90 minutes. When it goes off, stand up. Walk to the bathroom. Walk back. Do a slow lap if you can.
- If you can’t walk, sit and do calf raises: lift your heels off the floor, hold for 3 seconds, lower. Do 10 reps every 30 minutes.
- Flex your feet. Point your toes up toward your nose, then down. Repeat 20 times. This activates the muscle pump in your calves.
These aren’t suggestions. They’re evidence-backed actions. The CDC, ACCP, and IATA all agree: movement prevents clots. Period.
What About Extra Blood Thinners? Don’t Do It.
Some people think: “I’m on warfarin already. Maybe I should take aspirin too-or an extra dose.”
Don’t.
The ACCP 2021 guidelines say this clearly: adding aspirin or extra anticoagulants to prevent travel clots increases bleeding risk without proving any benefit. You’re not getting extra protection. You’re just increasing your chance of a bad bleed-inside your stomach, brain, or elsewhere.
There’s one exception: very high-risk travelers. If you’ve had an unprovoked clot before, or you’re actively undergoing cancer treatment, or had major surgery in the last 4 weeks, your doctor might prescribe a single dose of rivaroxaban 10mg or a low molecular weight heparin injection (like dalteparin) 1-2 hours before flying.
But that’s not for everyone. And it’s not something you decide on your own. Talk to your anticoagulation clinic or hematologist before your trip.
DOACs vs. Warfarin: Which Is Better for Travel?
If you’re choosing between anticoagulants, here’s the real difference:
| Feature | DOACs (e.g., rivaroxaban, apixaban) | Warfarin |
|---|---|---|
| Onset of action | 2 hours | 4-5 days |
| Monitoring needed? | No | Yes (INR blood test) |
| Diet restrictions | Minimal | Yes (vitamin K-rich foods) |
| Drug interactions | Fewer | Many |
| Cost (30 tablets, US) | $575 (rivaroxaban) | $4 (warfarin) |
| Travel practicality | Oral, no refrigeration | Requires INR testing abroad |
DOACs are easier for travel. No blood tests. No food rules. But they’re expensive. Warfarin is cheap, but you need to plan for INR checks. If you’re going to a country where labs don’t offer INR testing (many don’t), you’ll need a personal monitor like the Roche CoaguChek® Mobile-costing about $300 plus $7.50 per test strip.
Bottom line: DOACs win for convenience. Warfarin wins for cost. But if you’re on warfarin and traveling more than 2 weeks, bring your monitor.
What to Pack: Beyond Your Pills
Don’t just throw your meds in your carry-on. Pack smart:
- Original prescription bottles with your name and doctor’s info
- A printed copy of your most recent INR result (if on warfarin)
- A list of all medications: generic name, brand name, dose, frequency
- Contact info for your prescribing doctor
- A letter from your doctor explaining your condition and medication (in English and one other language if possible)
- Compression stockings
- Hydration: Bring a refillable water bottle. Avoid alcohol and sugary drinks-they dehydrate you and thicken your blood.
Also check if your medication is available at your destination. Apixaban? Not available in 32% of low-income countries, according to WHO data. If you’re going somewhere remote, bring extra. Don’t risk running out.
Warning Signs: Know When to Act
Clots don’t always show up during the flight. They can appear days or even weeks later.
Watch for these symptoms-any one of them needs urgent care:
- Swelling, pain, or warmth in one leg (72% of DVT cases start here)
- Sudden shortness of breath
- Chest pain that gets worse when you breathe
- Unexplained rapid heartbeat
- Coughing up blood
And don’t forget bleeding signs, especially if you’ve had a fall or injury:
- Bruising without cause
- Nosebleeds that won’t stop
- Bloody or black stools
- Red or brown urine
- Severe headache or dizziness
Carry emergency contact info for local hospitals at your destination. Save it in your phone and print a copy.
When Can You Fly After a Blood Clot?
If you had a DVT or PE recently, you’re probably scared to fly. The IATA 2020 Medical Manual says you can fly once you’re “asymptomatic and stable on anticoagulants.” That’s it. No time frame.
But Cambridge University Hospitals advises waiting at least 4 weeks. Why? Because your body is still healing. The clot hasn’t fully dissolved. The risk is highest in the first month.
So here’s the practical advice:
- Wait at least 4 weeks after diagnosis before flying.
- Get clearance from your hematologist.
- Use compression stockings.
- Walk every 2 hours.
- Don’t skip your meds.
If you’re unsure, don’t guess. Get a second opinion.
What’s Next? The Future of Travel and Clot Prevention
Research is moving fast. The MARVEL trial (NCT04585767), expected to finish in late 2024, is testing whether a specific DOAC dose can safely prevent travel-related clots in high-risk patients. If it works, we might soon have the first official drug protocol for this.
Right now, the best advice is simple: stay hydrated, move often, wear compression socks, take your meds on time, and know the warning signs. You don’t need to live in fear. You just need to be smart.
International travel on anticoagulants isn’t about avoiding the world. It’s about protecting yourself so you can keep exploring it.
Can I fly after having a blood clot?
Yes, but wait at least 4 weeks after diagnosis and only if you’re asymptomatic and stable on anticoagulant therapy. Always get clearance from your doctor first. Flying too soon increases the risk of another clot.
Should I take extra blood thinners before my flight?
No, unless your doctor specifically recommends it. For most people, adding aspirin or extra anticoagulants doesn’t prevent clots-it just raises your bleeding risk. Only very high-risk patients, like those with recent cancer or unprovoked clots, might need a single pre-travel dose of rivaroxaban or LMWH injection.
Is warfarin or a DOAC better for travel?
DOACs like rivaroxaban or apixaban are easier for travel-they don’t require blood tests, have fewer food interactions, and work faster. But they cost much more. Warfarin is cheap but needs INR monitoring. If you’re traveling longer than 2 weeks, consider bringing a personal INR monitor if you’re on warfarin.
Do compression stockings really help?
Yes. Medical-grade compression stockings (15-30 mmHg pressure) are proven to reduce DVT risk during long flights, especially for high-risk travelers. They’re not optional-they’re part of your safety plan. Wear them from the moment you leave home until you reach your destination.
Can I drink alcohol while on blood thinners during travel?
Avoid it. Alcohol dehydrates you and thickens your blood, increasing clot risk. It can also interfere with how warfarin works, making your INR unstable. Stick to water. It’s the safest choice for your circulation.
What if I run out of my blood thinner overseas?
Don’t risk it. Bring at least 10 days’ extra supply. Some DOACs aren’t available in low-income countries. Always carry a doctor’s letter and prescription in English and the local language. If you run out, contact your embassy or a local hospital-they may be able to help you get a short-term supply.






8 Comments