When your doctor prescribes a pill, they expect you to take it. But what happens when you don’t? For decades, doctors blamed patients for not following instructions. They called it compliance. Today, that language is outdated-and dangerous.
The Old Way: Compliance
Compliance means doing exactly what you’re told. No questions. No input. If your doctor says take two pills every morning, you take two pills every morning. If you miss one? You’re labeled non-compliant. Problem solved-right? Not even close. This approach assumes patients are passive. That they don’t have lives, jobs, kids, side effects, or bills. It ignores why someone might skip a dose: maybe the pill makes them nauseous, maybe they can’t afford it, maybe they forgot because they’re working two shifts. Compliance doesn’t ask why. It just counts pills. And it fails. A lot. The World Health Organization found that about half of people with chronic conditions stop taking their meds within the first year. Not because they’re stubborn. Because the system didn’t help them stay on track.The New Way: Adherence
Adherence is different. It’s not about obedience. It’s about partnership. The American Pharmacists Association defines adherence as: "the extent to which a patient’s behavior matches agreed-upon recommendations from a healthcare provider." Notice the word agreed-upon. That’s the key. Adherence means you and your doctor sit down, talk about what’s realistic. Maybe you can’t take a pill at 7 a.m. because you’re still asleep. So you switch to bedtime. Maybe the cost is too high-so you find a generic version or a patient assistance program. Maybe the side effects are worse than the disease-so you adjust the dose or try a different drug. Adherence doesn’t blame you for not following a plan that doesn’t fit your life. It asks: What’s stopping you? And here’s the science: patients who feel heard are 2.57 times more likely to stick with their treatment. That’s not magic. That’s human behavior.How They Measure the Difference
Compliance is simple: did you take the pill? Adherence is complex: did you start? Did you keep taking it? Did you stop because you felt better? Did you run out of money? Did you forget? Did you worry about long-term effects? Healthcare providers use several tools to track adherence:- Pill counts - counting leftover pills in the bottle
- Electronic caps - like MEMS, which record when you open your pill bottle
- Prescription refill records - seeing how often you refill your meds
- Self-reports - asking you directly, in a non-judgmental way
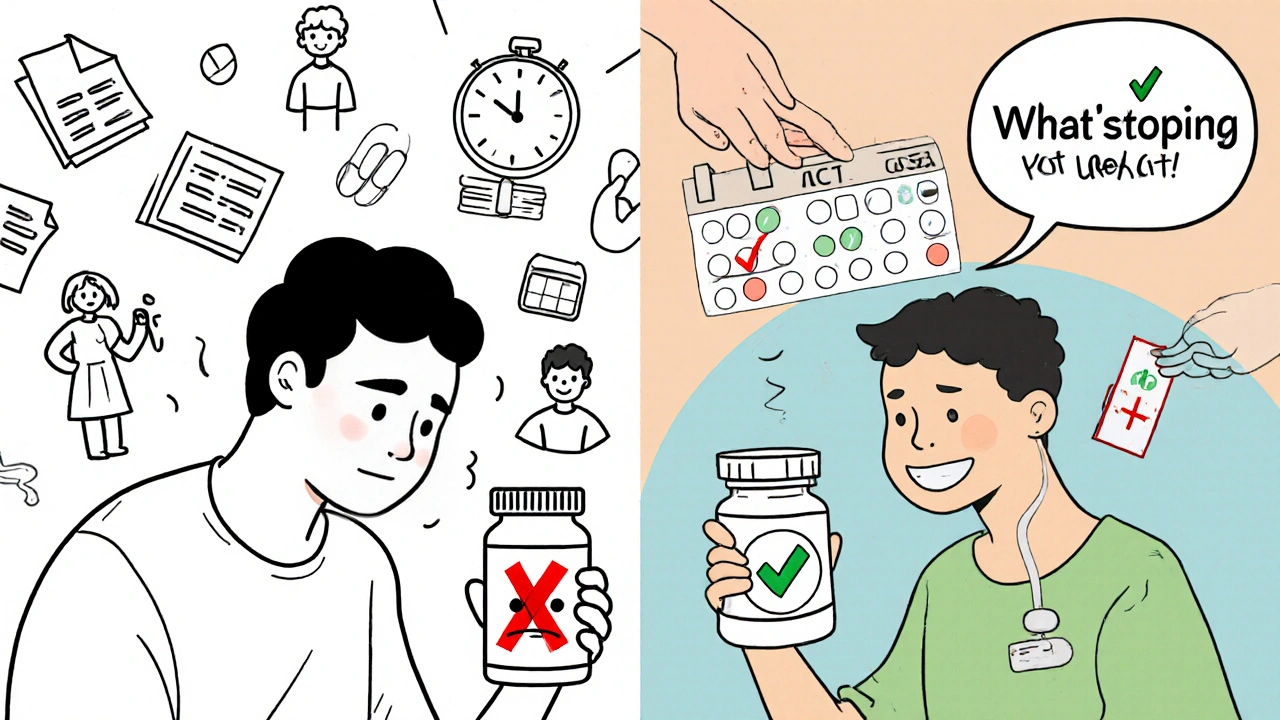
Why This Shift Changed Everything
In the 1990s, healthcare started moving away from “compliance.” Why? Because doctors realized patients weren’t the problem-the system was. A 2001 study in the Journal of Clinical Pharmacy and Therapeutics called compliance a “paternalistic relic.” By 2003, the Annals of Internal Medicine declared adherence the new standard. It wasn’t just a word change. It was a mindset shift. Think of it this way:- Compliance: “You must take this, or you’re failing.”
- Adherence: “Let’s figure out how to make this work for you.”
Real-World Impact: Who’s Doing It Right?
Some clinics are leading the way. Kaiser Permanente used a smart pill dispenser called Hero Health. It reminds patients when to take meds, tracks openings, and alerts nurses if doses are missed. Result? A 42% drop in missed doses. In a 2024 trial with 12,000 patients, Dose Packer’s tracking system boosted medication possession ratios by nearly 29%. That’s thousands of people staying on treatment longer. Even Medicare is catching on. Since January 2024, 8% of hospital payments are tied to how well patients stick to their meds. Hospitals now have a financial reason to help people adhere-not just punish them for failing. And it’s not just tech. It’s talk. Providers trained in motivational interviewing-asking open-ended questions, listening without judgment, helping patients set their own goals-see adherence rates jump by 37.6%. That’s not because they’re better doctors. It’s because they’re better listeners.What’s Holding Back the Change?
It’s not easy. Shifting from compliance to adherence takes time. A typical doctor visit is 15 minutes. Adding shared decision-making? That can stretch to 25. Many clinics don’t have the staff or the pay structure to support it. Some providers still think patients who skip meds are “non-compliant” or “difficult.” But research shows those labels are wrong. People don’t stop taking meds because they’re lazy. They stop because they’re scared, overwhelmed, or broke. And in some places-like prisons-compliance language still rules. The National Commission on Correctional Health Care found 63% of correctional facilities still use “compliance” in their policies. But even there, change is coming.
The Future Is Personal
The next big leap? AI. Google Health built a model that predicts, with 83.7% accuracy, who’s at risk of missing doses. It looks at 27 factors: income, education, past refill patterns, whether they live alone, even weather patterns. It doesn’t just say “you missed a dose.” It says, “You’re likely to miss your next dose because you’re out of refills and your bus schedule changed.” That’s not surveillance. That’s support. The American Medical Association added new billing codes in 2025 for adherence counseling (99487-99489). Now, doctors can get paid for having real conversations-not just writing prescriptions. The World Health Organization estimates that if adherence becomes the global standard, we could prevent 1 million premature deaths by 2030.What This Means for You
If you’re on medication-whether for high blood pressure, diabetes, depression, or anything else-this matters. You don’t have to be perfect. You don’t have to take every pill at the exact same minute. But you do deserve a plan that works with your life, not against it. Ask your doctor:- “Is there a cheaper version?”
- “Can I take this at night instead?”
- “What happens if I skip a dose?”
- “What side effects should I watch for?”
- “Can we adjust this if it’s not working?”






15 Comments