Medication Dry Eye Risk Calculator
This tool helps you assess your risk of medication-induced dry eyes and provides personalized recommendations based on the medications you're taking.
Medications You're Taking
Select all medications that apply to you
Why Your Medication Might Be Making Your Eyes Dry
You’re not imagining it. If your eyes feel gritty, burning, or like they’re full of sand-especially after starting a new pill-you’re not alone. Around 25-30% of all dry eye cases are caused by medications, and that number jumps to 40% for people over 65 who take multiple prescriptions. It’s not just aging. It’s what you’re taking.
Drugs don’t just target your symptoms-they can accidentally shut down your tear system. Your eyes need a steady mix of water, oil, and mucus to stay comfortable. When medications mess with any of those layers, your tear film breaks down. That’s when irritation starts.
Common Medications That Cause Dry Eyes
Some of the most widely used drugs are also the most likely to dry out your eyes. Here’s what’s on the list:
- Antihistamines like Benadryl, Claritin, and Zyrtec-designed to stop allergies-also block signals to your tear glands. They’re great for sneezing, terrible for your eyes.
- Antidepressants such as Zoloft, Prozac, amitriptyline, and nortriptyline reduce tear production by affecting nerve pathways. Many patients report dry eyes within weeks of starting these.
- Blood pressure meds like metoprolol, atenolol, and diuretics (Lasix, hydrochlorothiazide) pull fluid from your body, including your eyes. If you’re on a water pill, your eyes are likely paying the price.
- Glaucoma eye drops are a major culprit. Up to 47% of users get irritation from the preservative benzalkonium chloride (BAK). Switching to preservative-free versions cuts that risk in half.
- Isotretinoin (Accutane) for acne shuts down oil glands-including the ones in your eyelids that keep tears from evaporating. This one can cause long-term damage if not managed.
- Newer drugs like immune checkpoint inhibitors (used in cancer) and DPP-4 inhibitors for diabetes are now showing up in dry eye studies too.
It’s not always obvious. You might not connect your dry eyes to a medication you’ve been on for months. That’s why a simple question to your doctor-“Could this be causing my dry eyes?”-can change everything.
Lubrication That Actually Works
Not all eye drops are created equal. If you’re using preserved artificial tears more than four times a day, you’re probably making things worse. The preservatives in those bottles irritate your surface over time.
Switch to preservative-free drops. They come in single-use vials and are safe to use 4-6 times daily. Brands like Systane Ultra PF, Refresh Optive PF, and TheraTears Lubricant Eye Drops are widely recommended. Patients using these consistently report 78% symptom improvement when paired with glaucoma drops.
Here’s how to apply them right:
- Tilt your head back slightly.
- Use your finger to gently pull down your lower eyelid to make a small pocket.
- Hold the vial above your eye-don’t touch your eye or eyelid.
- Squeeze one drop in. Close your eye gently for 10 seconds.
Touching the tip to your eye risks contamination. And never apply eye drops right after your glaucoma drops. Wait at least 15 minutes. That way, both medications work properly.
Prescription Treatments When Drops Aren’t Enough
If over-the-counter drops aren’t cutting it, your eye doctor might recommend prescription options:
- Restasis (cyclosporine) reduces inflammation and helps your eyes make more tears. It takes 3-6 months to work, but users see a 15-20% increase in tear production.
- Xiidra (lifitegrast) works faster-often in 2-4 weeks-and reduces symptoms by 30% in clinical trials.
- Cequa is a newer version of cyclosporine with nanomicellar tech that boosts absorption by 300%. It’s pricier, but more effective for stubborn cases.
For severe dry eye, punctal plugs can help. These tiny devices block the tear ducts so your natural tears stay on the eye longer. Temporary collagen plugs last 3-6 months and work for 70% of patients. Silicone plugs are permanent and offer long-term relief.

Lifestyle Fixes That Make a Real Difference
Medication isn’t the only thing hurting your eyes. Your environment and habits play a huge role.
Use a humidifier. Keeping indoor humidity between 40-60% reduces tear evaporation by 25%. This is especially helpful in winter or in air-conditioned spaces.
Follow the 20-20-20 rule. Every 20 minutes, look at something 20 feet away for 20 seconds. This simple habit cuts digital eye strain by 35%-critical if you’re on antidepressants or antihistamines that already slow blinking.
Avoid direct airflow. Don’t sit in front of fans, car vents, or AC units. Air moving faster than 0.15 m/s over your face increases tear loss by 30%. Adjust your seat or use a shield.
Take omega-3s. A daily dose of 1,000-2,000 mg of EPA and DHA improves tear film stability in 60% of users within three months. Fish oil capsules or algae-based supplements work equally well. This helps most if you’re on diuretics or isotretinoin.
Quit smoking. Smoke irritates the eye surface and worsens dryness by 45%. Most people notice improvement in 2-4 weeks after quitting.
What to Do If Your Medication Can’t Be Stopped
Sometimes, you can’t stop the drug. Blood pressure meds, antidepressants, or cancer treatments are essential. But that doesn’t mean you’re stuck with dry eyes.
Work with your doctor to:
- Check if a lower dose helps. In 55% of cases, reducing the amount eases symptoms without losing effectiveness.
- Ask if there’s an alternative with fewer eye side effects. For example, some newer antidepressants (like bupropion) are less likely to cause dry eyes than SSRIs.
- Switch glaucoma drops to preservative-free versions. It’s a simple change with big results.
Never stop a medication on your own. Abruptly quitting blood pressure or antidepressant drugs can be dangerous. Always coordinate with both your prescribing doctor and your eye specialist.
When to See an Eye Specialist
See an optometrist or ophthalmologist if:
- Your dryness lasts more than two weeks despite using drops.
- You have pain, light sensitivity, or vision changes.
- Over-the-counter drops don’t help after 4 weeks.
Specialists now use tools like tear osmolarity tests and meibomian gland imaging to see exactly what’s going on. They can tell if your oil glands are blocked, your tears are too salty, or your nerves are damaged.
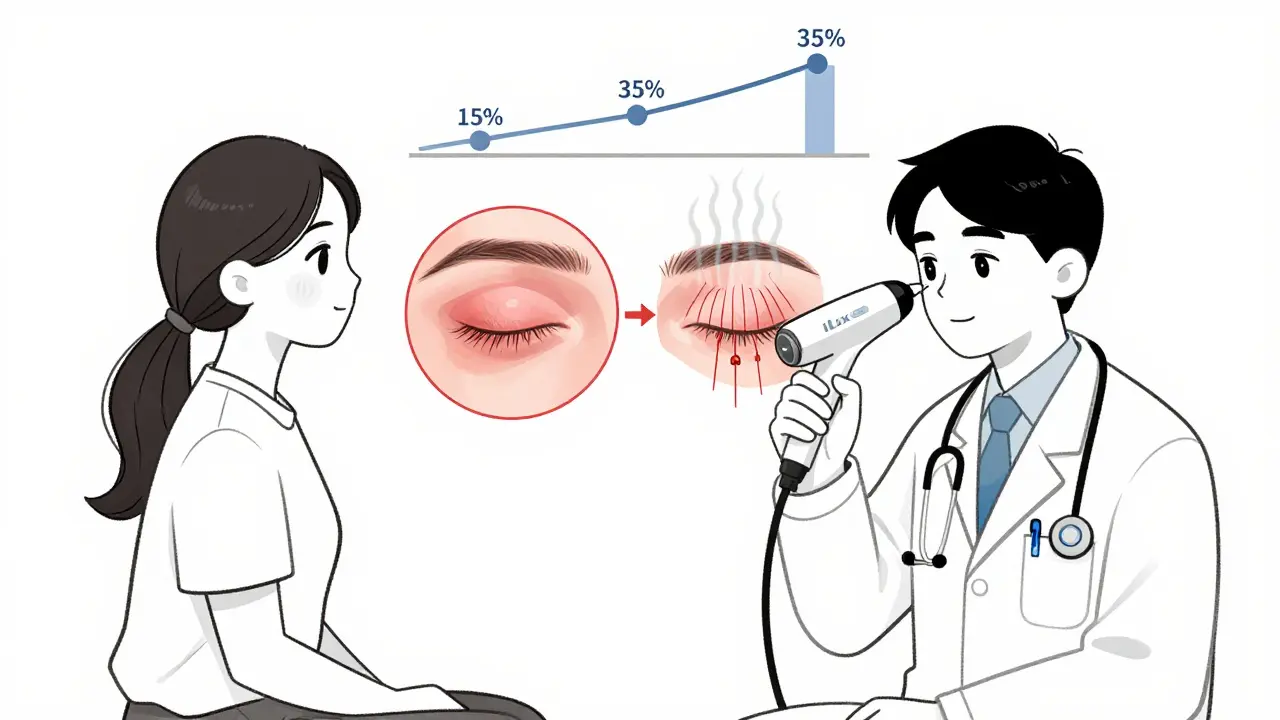
Thermal treatments like iLux (which heats and squeezes your eyelid glands) help 80% of patients with gland dysfunction-especially those on isotretinoin. It costs around $500 per session, but many find it life-changing.
Real People, Real Results
On Reddit’s dry eye community, users share what works:
- “After 3 months on Zoloft, my eyes felt like sandpaper. My optometrist recommended preservative-free Systane Ultra and warm compresses twice a day. Within two weeks, I could read for more than 20 minutes without burning.” - DryEyeWarrior2023
- “Isotretinoin wrecked my meibomian glands. Nothing helped until I tried iLux. Cost $500 per session, but I got 80% relief.” - AccutaneSurvivor
Most users report improvement within 2-4 weeks of sticking to a consistent routine. But patience matters. Prescription drops like Restasis take months. Lifestyle changes need time to build up.
What Not to Do
These mistakes make dry eye worse:
- Using preserved eye drops more than 4 times a day-preservatives add up and damage your surface.
- Applying artificial tears right after glaucoma drops-this washes away the medication.
- Ignoring redness or pain-dry eye can lead to corneal scratches if left untreated.
- Skipping follow-ups-your needs change as your meds or symptoms change.
What’s Changing in 2026
The field is evolving fast. In 2023, the FDA approved new preservative-free formulations, and by 2026, 35% of artificial tears sold are now preservative-free-up from just 15% in 2018.
Doctors are getting better at spotting medication-induced dry eye early. A 2023 NIH trial is testing a new lipid emulsion for isotretinoin users, with early results showing 40% improvement in tear stability after 8 weeks.
Experts predict a 25% drop in severe cases over the next five years as more prescribers check for eye side effects before writing prescriptions.
Final Thoughts
Dry eyes from medication aren’t just annoying-they’re common, treatable, and often reversible. You don’t have to live with burning, blurry vision just because you’re taking something for your health.
Start with the basics: switch to preservative-free drops, use a humidifier, take omega-3s, and follow the 20-20-20 rule. Talk to your doctor about alternatives or dose adjustments. And if it doesn’t improve in a few weeks, see an eye specialist.
Your eyes deserve more than a quick fix. With the right approach, you can protect your vision and keep your meds working-without the discomfort.








11 Comments