When you walk into a hospital or clinic and wait for hours just to see a doctor, it’s not just bad luck. It’s the result of a system breaking under the weight of its own shortages. Hospitals and clinics across the U.S. are running on fumes-staffed at 60-70% capacity, with nurses juggling five or six patients at a time, and emergency rooms so backed up that some patients wait over 72 hours. This isn’t a temporary spike. It’s a structural collapse that’s been building for years and is now hitting every corner of care.
Why the Staffing Crisis Is Worse Than You Think
The numbers don’t lie. By 2030, the U.S. will be short more than 500,000 registered nurses, according to the Health Resources and Services Administration. That’s not a guess-it’s a projection based on retirements, burnout, and not enough new nurses coming in. Nearly half of all nurses are over 50, and one-third will retire in the next decade. Meanwhile, nursing schools are turning away over 2,300 qualified applicants every year because they don’t have enough faculty to teach them.
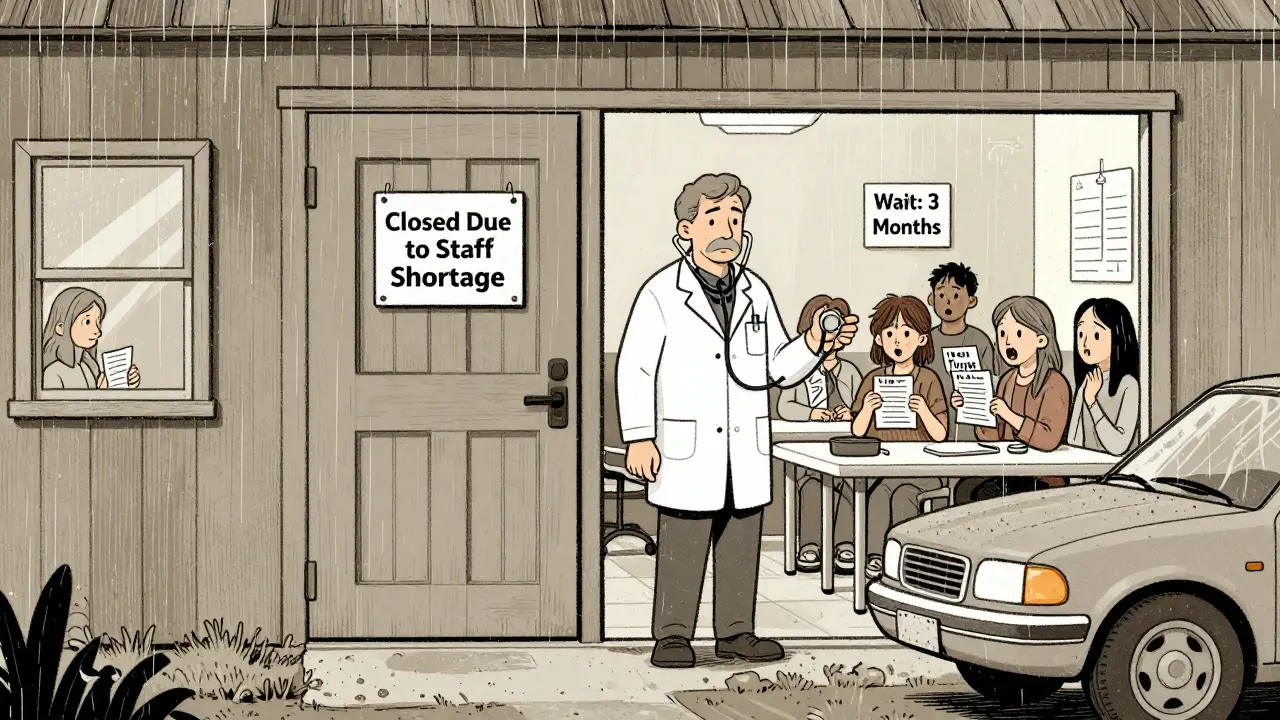
It’s not just nurses. Primary care doctors, mental health providers, and even medical assistants are in short supply. The Association of American Medical Colleges predicts an 86,000-physician shortfall by 2036. Rural areas are hit hardest: their hospitals operate with 37% more vacancies than urban ones. In places like rural Nevada or eastern Kentucky, clinics have closed outright because no one will work there. Even when they stay open, they’re running on borrowed time.
What Happens When There’s No One to Care for You
Staffing shortages don’t just mean longer wait times. They directly kill people. A 2022 study in JAMA found that hospitals with nurse-to-patient ratios higher than 1:4 saw 7% more deaths. That’s not a small difference-it’s the difference between life and death for hundreds of patients every week. In emergency departments, understaffing adds 22% to patient wait times. People with heart attacks, strokes, or severe infections are sitting in hallways while nurses scramble to keep up.
Medication errors are rising, too. ICU nurse Sarah Chen, who posted on Reddit in April 2025, said she recently made two near-miss errors because she was managing three critically ill patients alone. She wasn’t careless-she was exhausted. When nurses are stretched too thin, they skip checks. They rush med passes. They miss subtle signs of deterioration. The system isn’t just strained-it’s dangerous.
The Ripple Effect: Clinics, Long-Term Care, and Mental Health
It’s not just hospitals. Outpatient clinics are shutting down or cutting hours. A 2024 MGMA report showed rural clinics operating at just 58% staffing. That means fewer physicals, delayed screenings, and missed diagnoses. Diabetics aren’t getting their HbA1c checked. Cancer patients aren’t getting follow-ups. Preventable conditions turn into emergencies.
Long-term care facilities are even worse off. They’re 28% below pre-pandemic nursing levels, according to KFF. Residents with dementia are left unattended for hours. Pressure sores go untreated. Infections spread. Families are forced to choose between paying for private care or watching their loved ones deteriorate in understaffed nursing homes.
And then there’s mental health. The Department of Health and Human Services says we’ll be short over 12,400 behavioral health providers by 2025. That means people in crisis wait weeks for a therapy appointment-or end up in the ER, where there’s no real mental health support. One in five ER visits now involves a behavioral health issue. But there are no psychiatrists, no social workers, no beds. So patients sit in the ER for days, sometimes weeks, because no facility will take them.
Why the Band-Aids Aren’t Working
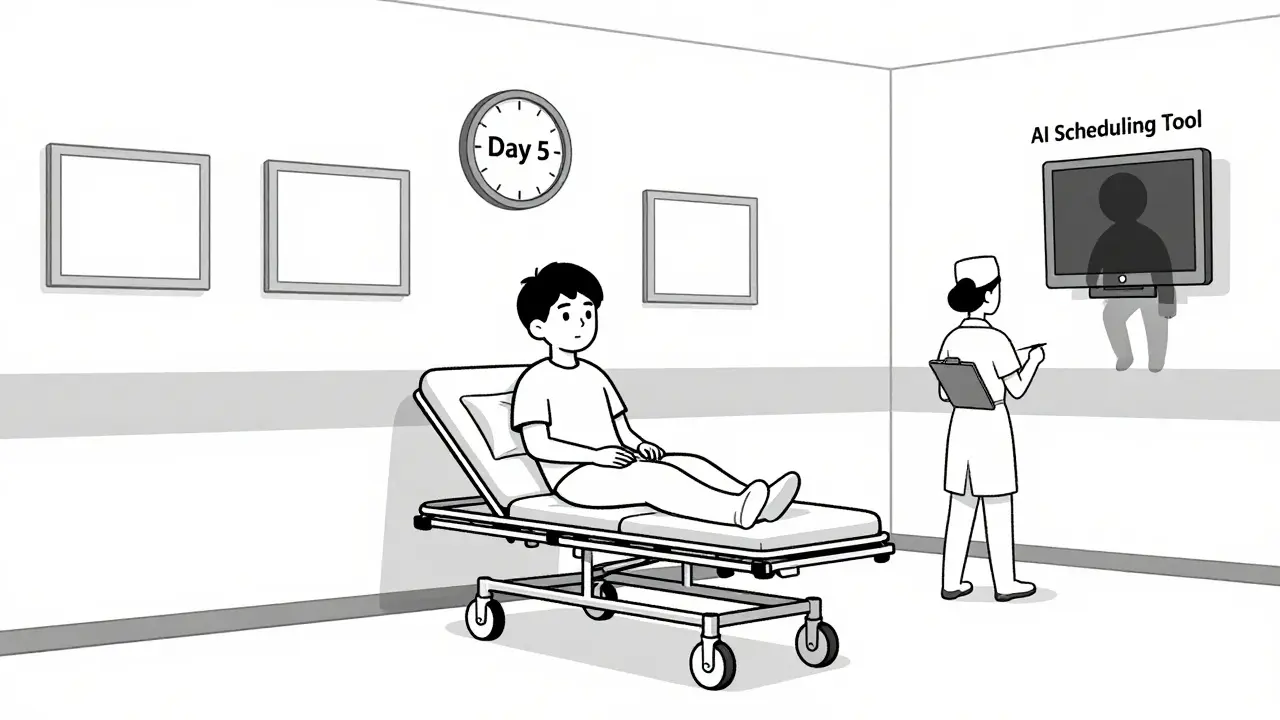
Hospitals have tried everything: hiring travel nurses, offering bonuses, using AI scheduling tools. But these are temporary fixes. Travel nurses fill 12% of open positions-but they cost 34% more than permanent staff. That’s why many hospitals are losing money even as they hire more people. The $185/hour travel nurse in New York makes six times what a hospital staff nurse makes. It’s creating resentment, not solutions.
AI tools promise to help with documentation and triage, but they’re slow to adopt. Clinicians need 32 hours of training just to use them. And 68% of hospitals say their electronic health records still don’t talk to each other, making telehealth and remote monitoring nearly impossible to scale.
States are trying too. California mandates nurse-to-patient ratios. Massachusetts offers loan forgiveness. But only 18 states have any staffing rules at all. And federal funding for nursing education? Just $247 million a year-when experts say we need $1.2 billion.
Who’s Getting Left Behind
The crisis isn’t equal. Rural patients, low-income communities, and elderly populations are hit hardest. A 65-year-old in rural West Virginia doesn’t have the option to drive 90 minutes to a better hospital. A single mother in Detroit can’t take three days off work to wait for a mental health appointment. People of color are more likely to live in areas with the fewest providers.
Even hospitals that are trying to do better are stuck. Magnet-designated hospitals-those with the best staffing and support-give nurses 4.2 hours of professional development each month. Non-Magnet hospitals? Just 1.1 hours. That gap isn’t just about money. It’s about whether the system values its people.
What Could Actually Fix This
There are real solutions-but they require investment, not just wishful thinking. We need to pay nurses what they’re worth. We need to fund nursing schools so they can hire more professors and accept more students. We need to remove state licensing barriers so nurses can move across state lines without waiting 112 days. We need to stop treating healthcare workers as disposable and start treating them as essential.
Technology can help, but only if it’s built for people, not profit. AI that reduces charting time by 30%? Great. AI that replaces human judgment? Dangerous. Telehealth that connects patients to therapists in 48 hours? Essential. Telehealth that cuts visits to save money? Harmful.
The Mayo Clinic’s Care Team Redesign took 18 months, $4.7 million, and hundreds of staff hours-but it cut nurse turnover by 31%. That’s proof it’s possible. But it’s not scalable unless we make it a national priority.
The Bottom Line
This isn’t just about hospitals running out of staff. It’s about a system that no longer works for patients, providers, or communities. Every delayed diagnosis, every extended ER wait, every medication error, every closed clinic is a consequence of choices we’ve made-or failed to make.
By 2030, 42 states will have nursing shortages. By 2036, we’ll be short tens of thousands of doctors. If we don’t act now, the damage won’t just be financial. It will be measured in lives lost, families broken, and trust shattered.
The healthcare system isn’t broken because of a pandemic. It was already cracked. The pandemic just showed us how deep the cracks go.
Why are hospitals so understaffed right now?
Hospitals are understaffed because nurses and doctors are leaving the field faster than they’re being replaced. Over half of nurses are over 50 and nearing retirement. Many quit due to burnout, unsafe patient ratios, and low pay. Nursing schools can’t train enough new nurses because they lack faculty. The pandemic accelerated these trends, but the problem started years before.
How do staffing shortages affect patient safety?
When nurses are assigned too many patients, mistakes happen. Studies show hospitals with nurse-to-patient ratios above 1:4 have 7% higher death rates. Medication errors, missed symptoms, and delayed treatments become more common. Emergency rooms see longer waits, which increases risk for stroke and heart attack patients. Staff exhaustion leads to lapses in care that can be fatal.
Are travel nurses helping solve the problem?
They’re filling gaps, but not solving the root issue. Travel nurses cover about 12% of open hospital positions, but they cost 34% more than permanent staff. This drives up hospital expenses and creates resentment among full-time staff who earn far less. It’s a short-term fix that makes financial strain worse and doesn’t increase the overall workforce.
Why can’t we just hire more nurses?
We can’t hire more because we don’t have enough training capacity. In 2023, nursing schools rejected over 2,300 qualified applicants due to lack of faculty. Teaching nursing requires experienced clinicians, but many are already working full-time in hospitals. Without more professors and funding for nursing education, we can’t grow the pipeline.
What’s being done to fix this?
Some states are mandating nurse-to-patient ratios. The Biden administration allocated $500 million for nursing education, but experts say we need $1.2 billion annually just to meet demand. Hospitals are trying AI tools and cross-training, but adoption is slow due to poor tech integration and staff resistance. Real progress requires systemic investment in education, pay, and working conditions-not just quick fixes.
Will telehealth help reduce the staffing shortage?
It can help in limited ways. Telehealth nurse triage has reduced ER visits by 19% in pilot programs. Remote monitoring can catch problems early. But 68% of hospitals can’t make these tools work because their electronic health records don’t communicate with each other. Plus, telehealth doesn’t replace in-person care for emergencies, surgeries, or chronic disease management. It’s a supplement, not a solution.




13 Comments