Elderly Diarrhea Risk Assessment Tool
Symptom Assessment
Please answer the following questions to assess your risk level for elderly diarrhea.
Risk Assessment Result
Key Takeaways
- Identify the most common triggers- infections, medication side effects, and chronic conditions.
- Watch for dehydration, blood, or fever as red‑flag signs that need medical attention.
- Start with fluid replacement and a bland diet; avoid anti‑diarrheal drugs unless advised.
- Review regular medicines, add probiotics or soluble fibre, and keep a symptom diary for long‑term control.
- Seek professional care promptly if symptoms persist beyond 48hours or worsen.
When it comes to gut health, Diarrhea in the Elderly is the frequent passage of loose stools in individuals aged 65 and older, often signaling underlying health issues. It isn’t just an inconvenience; rapid fluid loss can tip seniors into dehydration, electrolyte imbalance, and even hospitalization. Understanding why it happens and how to manage it effectively can keep older adults comfortable and safe at home.
Common Causes
Several factors converge in older adults, making diarrhea more likely than in younger people. Below is a quick rundown of the top culprits.
1. Infections
Pathogens such as Clostridioides difficile (often called C.difficile), norovirus, and certain bacteria thrive when the immune system weakens. Antibiotic‑associated diarrhea is especially common; broad‑spectrum antibiotics can wipe out good gut bacteria, allowing C.difficile to proliferate.
2. Medication Side Effects
Many prescription and over‑the‑counter drugs list diarrhea as a side effect. Common offenders include metformin, laxatives, iron supplements, and proton‑pump inhibitors. Polypharmacy-taking several medicines at once-raises the odds of a drug‑induced gut upset.
3. Food Intolerances and Diet Changes
Lactose intolerance, fructose malabsorption, and sudden increases in fiber can trigger loose stools. Seniors often switch to low‑fat or low‑sugar diets that lack adequate soluble fiber, upsetting the natural balance.
4. Chronic Diseases
Conditions like inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and uncontrolled diabetes can produce chronic diarrhea. Even heart failure or chronic kidney disease can lead to fluid shifts that manifest as watery stools.
5. Functional Changes with Age
Age‑related slowing of intestinal motility and reduced enzyme production make the gut more sensitive to irritants. This physiological shift, often called “senile gut,” can turn minor triggers into noticeable diarrhea.
Recognizing Warning Signs
Not all diarrhea is benign. Keep an eye out for these red‑flag symptoms, which suggest a deeper problem that requires prompt medical evaluation:
- Signs of Dehydration: dry mouth, dizziness, reduced urine output, or rapid heart rate.
- Visible blood or black/tarry stools, indicating possible bleeding.
- High fever (>38°C/100.4°F) or severe abdominal pain.
- Weight loss exceeding 5% over a short period.
- Diarrhea lasting longer than 48hours without improvement.
Immediate Management
When an older adult experiences an acute bout, start with the basics before reaching for medication.
- Fluid Replacement: Offer small sips of Oral Rehydration Solution (ORS) every 5‑10minutes. A homemade mix of water, a pinch of salt, and a teaspoon of sugar works well if commercial ORS isn’t on hand.
- Electrolyte Balance: Include a modest amount of clear broth or diluted fruit juice to restore potassium and sodium. Avoid pure water alone for prolonged periods, as it can dilute blood electrolytes.
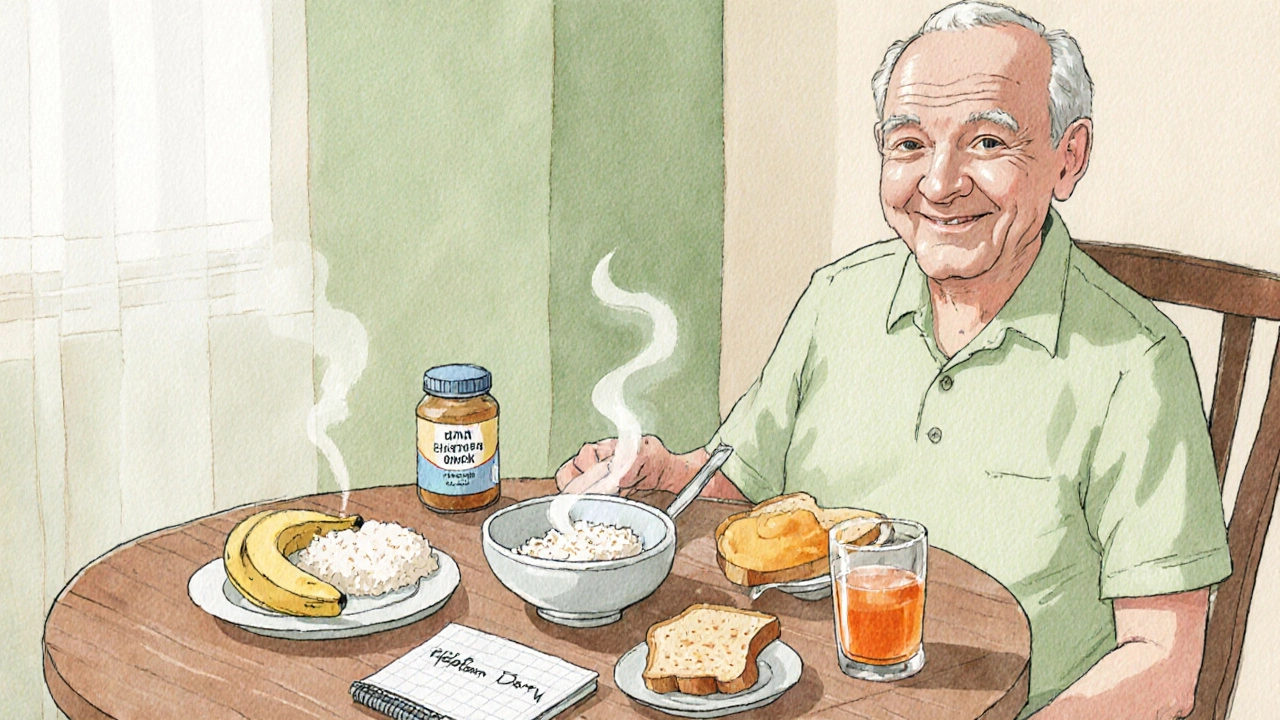
- Dietary Adjustments: Follow the BRAT diet (Bananas, Rice, Applesauce, Toast) for the first 24hours, then slowly reintroduce low‑fat, low‑fiber foods. Dietary Fiber, especially soluble types like oatmeal or psyllium, can firm stools once the gut settles.
- Medications: Over‑the‑counter loperamide (Imodium) can reduce stool frequency, but only if there’s no fever or bloody stool and the cause isn’t an infection. Always consult a pharmacist or doctor before using it in seniors.
- Probiotics: Strains such as Lactobacillus rhamnosus GG or Saccharomyces boulardii can shorten the course of antibiotic‑associated diarrhea. Choose a product with at least 5‑10billion CFU per dose.
Long‑Term Strategies
Preventing future episodes involves a combination of lifestyle tweaks and medical oversight.
- Medication Review: Schedule a yearly medication reconciliation with a physician or pharmacist. Identify drugs that may cause diarrhea and discuss alternatives or dose adjustments.
- Hydration Habits: Encourage regular fluid intake-about 1.5-2L per day, depending on kidney function and activity level. Flavor water with a splash of citrus or cucumber to make it more appealing.
- Smart Nutrition: Incorporate Probiotics through yogurt, kefir, or supplements. Add soluble fiber sources like oats, peeled apples, and bananas to bulk up stools without irritating the gut.
- Infection Prevention: Practice hand hygiene, especially after bathroom use or before meals. Ensure vaccinations for flu and rotavirus (where recommended) are up to date, as these infections can precipitate diarrhea.
- Screening & Monitoring: Regular Colon Cancer Screening (colonoscopy or FIT test) can catch early cancers that sometimes present with chronic diarrhea. Similarly, monitor blood glucose, thyroid function, and thyroid‑related hormones.
- Symptom Diary: Keep a simple log noting stool frequency, consistency (use the Bristol Stool Chart), foods eaten, and any new medications. Patterns can help clinicians pinpoint triggers.
When to Seek Professional Care
Even with diligent home care, some situations demand a clinician’s attention:
- Diarrhea persisting beyond 48hours despite fluid therapy.
- Presence of blood, mucus, or a dark tarry appearance.
- Fever≥38°C, severe abdominal cramping, or vomiting.
- Signs of severe dehydration: confusion, rapid pulse, or low blood pressure.
- Recent hospitalization or antibiotic use, which raises suspicion for C.difficile infection.
In these cases, a stool culture, C.difficile toxin assay, or imaging may be ordered to guide treatment.

Quick Reference Checklist
- ► Assess hydration status every 2hours.
- ► Offer ORS or clear broth; avoid caffeine and alcohol.
- ► Introduce bland foods; add soluble fiber after 24hours.
- ► Review all current medicines for diarrheal side effects.
- ► Consider probiotic supplement (5‑10billion CFU).
- ► Seek medical help if red‑flag signs appear or symptoms last >48hours.
Comparison of Common Causes and First‑Line Management
| Cause | Typical Onset | First‑Line Management |
|---|---|---|
| Antibiotic‑associated (C. difficile) | 2‑7days after antibiotic start | Stop offending antibiotic, start oral vancomycin or fidaxomicin; aggressive ORS |
| Medication side effect | Hours to days after new drug | Review meds with doctor, adjust or discontinue culprit |
| Viral gastroenteritis (norovirus) | 12‑48hours after exposure | Hydration, rest, avoid anti‑diarrheals if fever present |
| Food intolerance (lactose, fructose) | Minutes to hours after meal | Eliminate offending sugar, introduce lactase enzyme if needed |
| IBD flare | Variable, often weeks | Prescription anti‑inflammatory meds, diet low‑residue, specialist follow‑up |
Frequently Asked Questions
What is the safest fluid for rehydrating an elderly person with diarrhea?
A balanced oral rehydration solution containing sodium, potassium, glucose, and a small amount of bicarbonate is ideal. If commercial ORS isn’t available, a homemade mix of 1liter water, 6teaspoons sugar, and half a teaspoon salt works well.
Can over‑the‑counter anti‑diarrheal pills be used in seniors?
They can be used only if there’s no fever, blood in the stool, or suspicion of an infection. Loperamide should be avoided in cases of C.difficile or severe constipation risk.
How long should I monitor a diarrhea episode before calling a doctor?
If symptoms persist beyond 48hours, worsen, or are accompanied by red‑flag signs like dehydration, blood, or high fever, seek medical care immediately.
Do probiotics really help prevent recurrence?
Clinical studies show that daily probiotics, especially strains such as Lactobacillus rhamnosus GG or Saccharomyces boulardii, can reduce the duration of antibiotic‑associated diarrhea by up to 40% and lower recurrence rates.
Is a low‑fiber diet advisable for seniors with diarrhea?
In the acute phase, a low‑residue, low‑fiber diet helps to firm stools. Once the episode resolves, reintroducing soluble fiber gradually supports regular bowel movements without aggravating symptoms.








10 Comments